Book Appoinment
Thyroid Cancer
Thyroid cancer develops in your thyroid gland, a part of your endocrine system. Your thyroid gland produces hormones that regulate body temperature, heart rate and metabolism. Most thyroid cancers are highly curable. Treatments include surgery, chemotherapy, radiation, hormone therapy and radioiodine therapy.
Overview
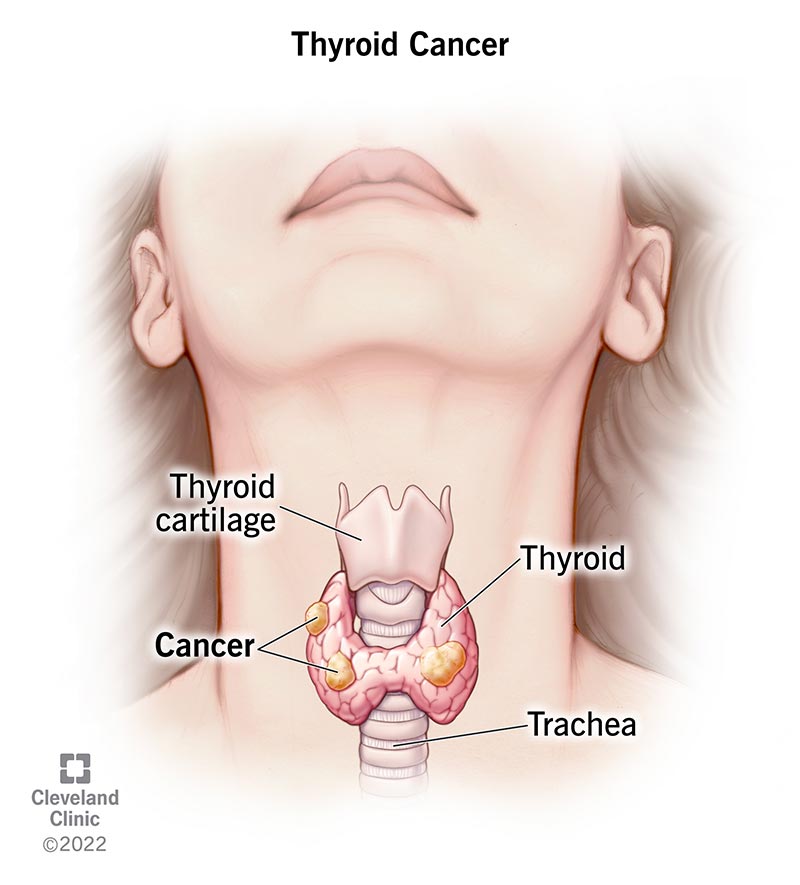
What is thyroid cancer?
Thyroid cancer develops in your thyroid, a small, butterfly-shaped gland at the base of your neck. This gland produces hormones that regulate your metabolism (how your body uses energy). Thyroid hormones also help control your body temperature, blood pressure and heart rate. Thyroid cancer, a type of endocrine cancer, is generally highly treatable, with an excellent cure rate.
How common is thyroid cancer?
Close to 53,000 Americans receive a thyroid cancer diagnosis every year. Treatments for most thyroid cancers are very successful. Still, about 2,000 people die from the disease every year.
Women and people assigned female at birth (AFAB) are three times more likely to get thyroid cancer compared to men and people assigned male at birth (AMAB). The disease is commonly diagnosed in women and people AFAB in their 40s and 50s and men and people AMAB in their 60s and 70s. Even children can develop the disease.
What are the types of thyroid cancer?
Healthcare providers classify thyroid cancer based on the type of cells from which the cancer grows. Types of thyroid cancer include:
- Papillary: Up to 80% of all thyroid cancers are papillary. This cancer type grows slowly. Although papillary thyroid cancer often spreads to lymph nodes in your neck, the disease responds very well to treatment. Papillary thyroid cancer is highly curable and rarely fatal.
- Follicular: Follicular thyroid cancer accounts for up to 15% of thyroid cancer diagnoses. This cancer is more likely to spread to your bones and organs, like your lungs. Metastatic cancer (cancer that spreads) may be more challenging to treat.
- Medullary: About 2% of thyroid cancers are medullary. A quarter of people with medullary thyroid cancer have a family history of the disease. A faulty gene (genetic mutation) may be to blame.
- Anaplastic: This aggressive thyroid cancer is the hardest type to treat. It can grow quickly and often spreads into surrounding tissue and other parts of your body. This rare cancer type accounts for about 2% of thyroid cancer diagnoses.
What are the thyroid cancer stages?
Healthcare providers use a staging system to determine if and how far thyroid cancer has spread. Generally, when cancer cells in your thyroid metastasize, they spread to your nearby structures and lymph nodes first. After that, the cancer can spread to distant lymph nodes, organs, and bones.
Thyroid cancer stages range from 1 (I) to 4 (IV). In simple terms, the higher the number, the more the cancer has spread. To learn more about cancer staging and how it applies to your specific diagnosis, talk to your healthcare provider.
Symptoms and Causes
What are the warning signs of thyroid cancer?
You or your healthcare provider might feel a lump or growth in your neck called a thyroid nodule. Don’t panic if you have a thyroid nodule. Most nodules are benign (not cancer). Only about 3 out of 20 thyroid nodules turn out to be cancerous (malignant).
Other thyroid cancer symptoms include:
- Difficulty breathing or swallowing.
- Loss of voice (hoarseness).
- Swollen lymph nodes in your neck.
What are the signs that thyroid cancer has spread?
If you have thyroid cancer that has spread (metastasized) to other areas of your body, you may experience symptoms such as:
- Tiredness.
- Loss of appetite.
- Nausea and vomiting.
- Unexpected weight loss.
What causes thyroid cancer?
Experts aren’t sure why some cells become cancerous (malignant) and attack your thyroid. Certain factors, such as radiation exposure, a diet low in iodine, and faulty genes can increase risk. Other risk factors include:
- Enlarged thyroid (goiter).
- Family history of thyroid disease or thyroid cancer.
- Thyroiditis (inflammation of your thyroid gland).
- Gene mutations (changes) that cause endocrine diseases, such as multiple endocrine neoplasia type 2A (MEN2A) or type 2B (MEN2B) syndrome.
- Low iodine intake.
- Obesity (high body mass index).
- Radiation therapy for head and neck cancer, especially during childhood.
- Exposure to radioactive fallout from nuclear weapons or a power plant accident.
Diagnosis and Tests
How is thyroid cancer diagnosed?
If you have an enlarged thyroid nodule or other signs of thyroid cancer, your healthcare provider may order one or more of these tests:
- Blood tests: A thyroid blood test checks hormone levels and gauges whether your thyroid is functioning properly.
- Biopsy: During a fine-needle aspiration biopsy, your healthcare provider removes cells from your thyroid to test for cancer cells. A sentinel node biopsy can determine if cancer cells have spread to lymph nodes. Your provider may use ultrasound technology to guide these biopsy procedures.
- Radioiodine scan: This test can detect thyroid cancer and determine if cancer has spread. You swallow a pill containing a safe amount of radioactive iodine (radioiodine). Over a few hours, your thyroid gland absorbs the iodine. Your healthcare provider uses a special device to measure the amount of radiation in the gland. Areas with less radioactivity need more testing to confirm the presence of cancer.
- Imaging scans: Radioactive iodine scan, computed tomography (CT) and positron emission tomography (PET) scans can detect thyroid cancer and cancer spread.
Management and Treatment
How is thyroid cancer managed or treated?
Treatments for thyroid cancer depend on the tumor size and whether the cancer has spread. Treatments include:
- Surgery: Surgery is the most common treatment for thyroid cancer. Depending on the tumor’s size and location, a surgeon may remove part of your thyroid gland (lobectomy) or all of the gland (thyroidectomy). The surgeon also removes any nearby lymph nodes where cancer cells have spread.
- Radioiodine therapy: With radioiodine therapy, you swallow a pill or liquid containing a higher dose of radioactive iodine than what’s used in a diagnostic radioiodine scan. The radioiodine shrinks and destroys the diseased thyroid gland along with cancer cells. This treatment is very safe. Your thyroid gland absorbs almost all of the radioiodine and the rest of your body has minimal radiation exposure.
- Radiation therapy: Radiation kills cancer cells and stops them from growing. External radiation therapy uses a machine to deliver strong beams of energy directly to the tumor site. Internal radiation therapy (brachytherapy) involves placing radioactive seeds in or around the tumor.
- Chemotherapy: Intravenous or oral chemotherapy drugs kill cancer cells and stop cancer growth. Very few people diagnosed with thyroid cancer will ever need chemotherapy.
- Hormone therapy: This treatment blocks the release of hormones that can cause cancer to spread or come back.
What are the complications of thyroid cancer?
Thyroid cancer can spread (metastasize) to other parts of your body, such as your liver, lungs or bones. Detecting and treating thyroid cancer in the early stages reduces your risk for metastasis.
Thyroid cancer can recur (come back), even after treatment. Because thyroid cancer grows slowly, it could take up to 20 years to come back. Recurrence happens in up to 30% of thyroid cancer cases.
Overall, thyroid cancer prognosis (outlook) is positive. But it’s important to know that after thyroid surgery or treatments, your body still needs thyroid hormones to function. You’ll need thyroid replacement hormone therapy for life. Synthetic thyroid hormones, such as levothyroxine (Synthroid®), take over for the thyroid hormones that your body no longer naturally produces.
How does thyroid cancer affect pregnancy?
Thyroid cancer is the second most common cancer diagnosed in people who are pregnant (breast cancer is first). Approximately 10% of thyroid cancers develop during pregnancy or within the first year after childbirth. Experts believe fluctuating hormone levels during pregnancy may trigger the cancer.
If you receive a thyroid cancer diagnosis during pregnancy, your healthcare provider can discuss treatment options. Depending on the cancer type and severity, your provider may recommend delaying treatment until after you deliver your baby. If treatment can’t wait, most people can safely undergo surgery to remove the cancerous gland. You shouldn’t have radioactive diagnostic tests or treatments when you’re pregnant or breastfeeding (chestfeeding).
How long does it take to recover from thyroid cancer treatment?
Recovery depends on several factors, including your age, the size and stage of your thyroid tumor, and what type of treatment you received. Talk to your healthcare provider about what to expect during and after your thyroid cancer treatment.
Prevention
Can I prevent thyroid cancer?
Many people develop thyroid cancer for no known reason, so prevention isn’t really possible. But if you know you’re at risk for thyroid cancer, you may be able to take these steps:
- Preventive (prophylactic) surgery: Genetic tests can determine if you carry an altered gene (a mutation) that increases your risk for medullary thyroid cancer or multiple endocrine neoplasia. If you have the faulty gene, you may opt to have preventive (prophylactic) surgery to remove your thyroid gland before cancer develops.
- Potassium iodide: If you’ve had radiation exposure during a nuclear disaster, such as the 2011 incident at Fukushima, Japan, taking potassium iodide within 24 hours of exposure can lower your risk of eventually getting thyroid cancer. Potassium iodide (Pima®) blocks your thyroid gland from absorbing too much radioiodine. As a result, your gland stays healthy.
Outlook / Prognosis
What’s the thyroid cancer survival rate?
Eight out of 10 people who have thyroid cancer develop the papillary type. Papillary thyroid cancer has a five-year survival rate of almost 100% when the cancer is in their gland (localized). Even when the cancer spreads (metastasizes), the survival rate is close to 80%. This rate means that, on average, you’re about 80% as likely to live for at least five years after diagnosis as someone who doesn’t have metastatic papillary thyroid cancer.
Five-year survival rates for other thyroid cancer types include:
- Follicular: Close to 100% for localized; around 63% for metastasized.
- Medullary: Close to 100% for localized; around 40% for metastasized.
- Anaplastic: Close to 31% for localized; 4% for metastasized.
Is thyroid cancer curable?
Yes, most thyroid cancers are curable with treatment, especially if the cancer cells haven’t spread to distant parts of your body. If treatment doesn’t fully cure thyroid cancer, your healthcare provider can design a treatment plan to destroy as much of the tumor as possible and prevent it from growing back or spreading.
Living With
When should I see my healthcare provider?
You should call your healthcare provider if you have thyroid cancer and you experience:
- Lump in your neck.
- Rapid heart rate.
- Unexplained weight loss or gain.
- Extreme fatigue.
What questions should I ask my doctor?
If you have thyroid cancer, you may want to ask your healthcare provider:
- Why did I get thyroid cancer?
- What type of thyroid cancer do I have?
- Has the cancer spread outside of my thyroid gland?
- What’s the best treatment for this type of thyroid cancer?
- What are the treatment risks and side effects?
- Will I need thyroid replacement hormone therapy?
- Is my family at risk for developing this type of thyroid cancer? If so, should we get genetic tests?
- Can I get thyroid cancer again?
- Am I at risk for other types of cancer?
- What type of follow-up care do I need after treatment?
- Should I look out for signs of complications?