Book Appoinment

Cervical Cancer
Cervical cancer is cancer of the cells in your cervix. HPV infections cause most cervical cancers. Getting Pap tests and practicing safe sex are the most important steps you can take to help prevent cervical cancer. Surgery, radiation and chemotherapy are the main treatments for cervical cancer.
Overview
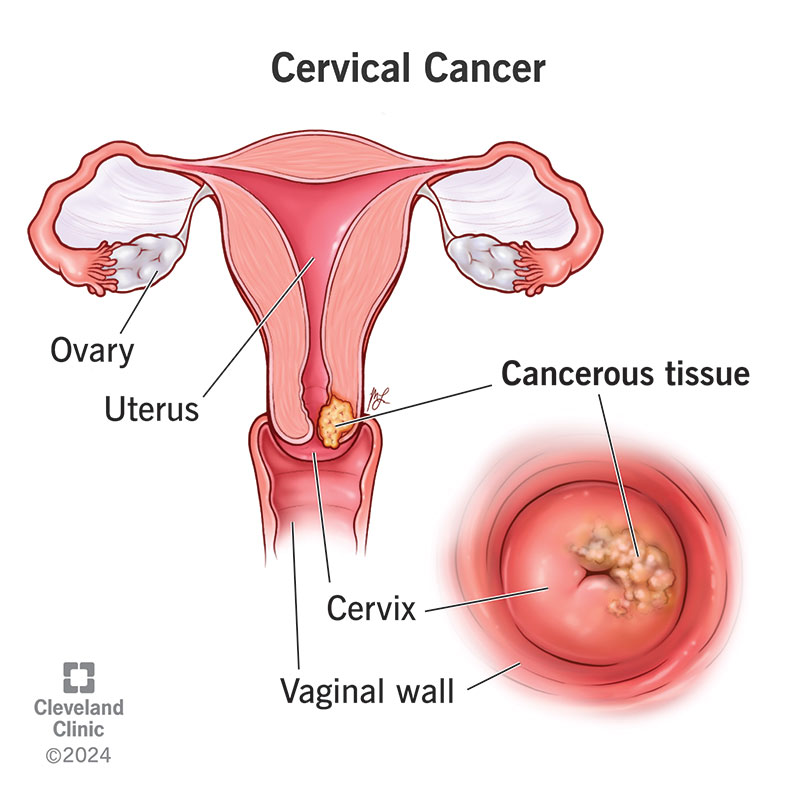
What is cervical cancer?
TCervical cancer is cancer that begins on the surface of your cervix. It happens when the cells on your cervix start to change to precancerous cells. HPV (human papillomavirus) infection causes almost all cases of cervical cancer. HPV is a virus that spreads through sexual contact. You can lower your risk of cervical cancer by getting regular cervical cancer screenings (like a Pap smear) and receiving the HPV vaccine.
Cervical cancer often doesn’t cause symptoms until it begins to spread. That’s why regular screenings and the HPV vaccine are so important. Cervical cancer is highly treatable when found in the early stages. A healthcare provider can treat it with surgery, radiation therapy, chemotherapy and other cancer medications.
About 14,000 people in the United States receive a cervical cancer diagnosis each year. Women and people assigned female at birth (AFAB) between the ages of 35 and 44 are most likely to receive a diagnosis.
Types of cervical cancer
There are two main types of cancer of the cervix: squamous cell carcinomas and adenocarcinomas. About 80% to 90% of cervical cancers are squamous cell carcinomas, while 10% to 20% are adenocarcinomas. You can also have a mix of both types.
Symptoms and Causes
What are the warning signs of cervical cancer?
Early stages of cervical cancer don’t usually involve symptoms and are hard to detect. The first signs of cervical cancer may take time to develop.
Signs and symptoms of Stage I cervical cancer can include:
- Watery or bloody vaginal discharge that may be heavy and can have a foul odor.
- Vaginal bleeding after sex, between menstrual periods, or after menopause.
- Pain during sex (dyspareunia).
If cancer has spread to nearby tissues or organs, symptoms may include:
- Difficult or painful urination, sometimes with blood in urine.
- Diarrhea, or pain or bleeding from your rectum when pooping.
- Fatigue, loss of weight, and appetite.
- A general feeling of illness.
- Dull backache or swelling in your legs.
- Pelvic/abdominal pain.
If you experience abnormal bleeding, unusual vaginal discharge, or any other unexplainable symptoms, you should contact a healthcare provider.
What causes cervical cancers
Most cervical cancers are caused by HPV, a sexually transmitted infection. HPV spreads through sexual contact (anal, oral or vaginal) and can lead to cancer. Most people will get HPV at some point in their lives and not realize it because their bodies fight the infection. But if your body doesn’t fight the infection, it can cause the cells of your cervix to change to cancerous cells.
HPV and cervical cancer
There are more than 100 kinds of HPV and about a dozen of them have been shown to lead to cancer. Early detection of these HPV strains is key in preventing cervical cancer. The HPV vaccine can help prevent HPV infection by protecting you against the HPV that causes up to 90% of all cervical cancers.
Who’s at risk for cervical cancer?
In many cases, you can have no known risk factors for cervical cancer. Other times, you have one or more risk factors. Some risk factors within your control are:
- Screening history: People who haven’t had Pap tests at regular intervals are more likely to get cervical cancer (because Pap tests can detect precancerous cells).
- HPV infection: Certain types of HPV cause cervical cancer. Lowering your risk for HPV can also lower your risk for cervical cancer.
- Sexual history: Having sexual intercourse before the age of 18 and having many sexual partners may put you at higher risk of HPV infection.
- Smoking: Smoking cigarettes increases your risk of cervical cancer.
- HIV infection: People with HIV have a higher-than-average risk of developing cervical cancer.
- Having a weakened immune system: Having a weak immune system makes your body unable to fight infections.
There are some risk factors you can’t change or control. These are:
- DES (diethylstilbestrol): DES is a medication that was given to people between 1938 and 1971 to prevent miscarriage. If your birth parent took DES, you may be more likely to get cervical cancer.
- Family history: Cervical cancer may have a genetic component.
How long can cervical cancer go unnoticed?
Precancerous cell changes can progress slowly, but once it turns into cancer, it can progress quickly. It takes between three and seven years for abnormal cell changes to become cancer. Pap tests can detect precancerous cell changes before they have a chance to turn into cancer. If you’re keeping up with regular Pap tests, cervical cancer isn’t likely to go unnoticed.
What are complications of cervical cancer?
Early detection and treatment of cervical cancer are key to avoiding life-threatening complications of the disease. That’s why regular Pap smears and HPV tests are critical.
Some possible complications of cervical cancer include:
- Pain: Cancer can be painful when it spreads.
- Bladder and bowel changes: Cervical cancer can cause urinary problems like difficulty peeing. It can also cause constipation.
- Kidney damage: Kidney failure is a complication of advanced cervical cancer.
- Blood clots: Your risk for blood clots increases because blood becomes “sticky” when you have cancer. This may slow your blood flow and lead to a clot developing.
- Bleeding: You may experience bleeding from your vagina, rectum, or bladder if cancer spreads to those organs.
- Fertility or pregnancy challenges: Depending on the treatment you have, you could lose the ability to get pregnant. Surgery on your cervix to remove cancer cells could also increase your chance of miscarriage with future pregnancies.
- Side effects of cancer treatment: Chemotherapy, radiation, and other cancer treatments can cause unpleasant side effects like nausea and vomiting, fatigue, and sexual dysfunction.
Diagnosis and Tests
How is cervical cancer diagnosed?
Cervical cancer usually develops slowly and over many years. Before turning into cancer, the cells in your cervix go through a lot of changes. The once normal cells in your cervix start to appear irregular or abnormal. These abnormal cells may go away, stay the same or turn into cancer cells.
Regular cervical cancer screenings with a Pap test can detect most cases of cervical cancer. The goal of cervical cancer screening is to detect cell changes on your cervix before they become cancer. A Pap test, or Pap smear, involves looking at cells from your cervix under a microscope. These cells are examined for signs of precancers or other irregularities.
If your Pap comes back as abnormal, further testing is necessary. This could include an HPV test, which is a specific test that checks the cells of your cervix for the HPV strains that are most likely to cause cancer.
Tests to diagnose cervical cancer
If your screenings come back as abnormal, your healthcare provider will want to run more tests to confirm you have cervical cancer. The first step in that is typically a colposcopy. A colposcope magnifies the cells of your cervix so your healthcare provider can see irregular cells. If the cells look suspicious or unusual, they’ll remove a sample of cervical cells and send them to a lab for further testing.
They can use any of the following methods to get a sample of tissue from your cervix:
- Punch biopsy: Your provider uses a cutting tool with a round top to cut out the precancerous cells.
- Endocervical curettage: A procedure that involves your provider scraping the lining of your cervix with a spoon-shaped tool called a curette.
- Loop electrosurgical excision procedure (LEEP): Your provider uses an electrical wire loop to remove the abnormal cervical tissue.
- Cone biopsy: Your provider removes a slightly larger, cone-shaped piece of tissue from your cervix.
If the results from these test confirms cervical cancer, further tests will determine whether the disease has spread (metastasized). These tests might include:
- Liver and kidney function studies.
- Blood and urine tests.
- X-rays of your bladder, rectum, bowels, and lungs.
- CT scans.
- MRI.
The results of these tests also help your healthcare provider stage the cancer. Cervical cancer ranges from Stage I (least severe) to Stage IV (most severe). Staging helps your healthcare provider determine the best treatment plan.
What are the stages of cervical cancer?
There are four main stages of cervical cancer, and within each stage, there can be several different substages. The main stages of cervical cancer are:
- Stage I: Cancer is found only in the neck of your cervix. It hasn’t spread to the deeper parts of your cervical tissue.
- Stage II: Cancer has spread beyond your cervix and uterus but hasn’t yet spread to your pelvic wall (the tissues that line the part of the body between your hips) or your lower vagina.
- Stage III: Cancer has spread to the lower part of your vagina and may have spread to your pelvic wall, ureters (tubes that carry pee from your kidneys to your bladder) and nearby lymph nodes.
- Stage IV: Cancer has spread to your bladder, rectum or other parts of the body like your bones or lungs.
Your healthcare provider is the best person to discuss what stage of cervical cancer you have and what it means.
What does cervical cancer look like?
Cervical cancer cells look different under a microscope compared to normal or healthy cells. Only a pathologist can identify these changes. You wouldn’t be able to see or touch cervical cancer on your own. A pathologist will notice the following features of cervical cancer cells:
- Different size and shape.
- Loss of structure or organization.
- Increase in fluid inside the cell.
- A darkened center.
Management and Treatment
How is cervical cancer treated?
The cervical cancer treatment team includes a gynecologic oncologist. Treatment for cervical cancer is based on many factors, including the stage of the disease, your age and general health, and if you want children in the future.
The treatments for cervical cancer are radiation, chemotherapy, surgery, targeted therapy and immunotherapy.
Clinical trials are another treatment option. They’re controlled research studies to test new treatments for cancer. Talk to your oncologist if you’d like to participate in a clinical trial.
Some people use alternative treatments like diet, herbs, acupuncture and other methods to supplement their cancer treatment. Talk to your healthcare provider about alternative methods that claim to relieve cancer symptoms. Some may help, but others could be harmful.
Radiation
Radiation therapy uses energy beams to kill cancer cells on your cervix. There are two types of radiation therapy:
- External beam radiation therapy (EBRT): Aims high-powered radiation at cancer from a machine outside your body.
- Brachytherapy: Puts the radiation in or just near cancer.
Chemotherapy
Chemotherapy (chemo) uses drugs injected into your veins or taken by mouth to kill cancer cells. It enters your blood and is effective for killing cells anywhere in your body. There are several drugs used for chemo and they can be combined. Chemo is often given in cycles. The length of the cycle and the schedule or frequency of chemotherapy varies depending on the drug used and where the cancer is in your body.
Surgery
Different kinds of surgery are used to treat cervical cancer. Your provider can remove just the cancerous tissues when the cancer is in its early stages. Some of the most common kinds of surgery for cervical cancer include:
- Laser surgery: This surgery uses a laser beam to burn off just the cancer cells.
- Cryosurgery: This surgery freezes cancer cells, destroying them.
- Hysterectomy: This surgery involves the removal of your uterus and cervix.
- Trachelectomy: This procedure removes your cervix and the upper part of your vagina but not your uterus.
- Pelvic exenteration: This is the same as a hysterectomy but also includes your bladder, vagina, rectum, and part of your colon, depending on where the cancer has spread.
Some people may have a combination of treatments. Your provider may use radiation or chemotherapy to treat cancer that has spread or come back (recurred). Sometimes, your provider will use radiation and chemotherapy before or after surgery.
Targeted therapy
Targeted drug treatment destroys specific cancer cells without damaging healthy cells. It works by targeting proteins that control how cancer cells grow and spread. As scientists learn more about cancer cells, they’re able to design better-targeted treatments that destroy these proteins.
Immunotherapy
Immunotherapy uses medicine to stimulate your immune system to recognize and destroy cancer cells. Cancer cells pretend to be healthy to hide from your immune system. Immunotherapy helps target these signals so the cancer cells can’t trick your body into thinking it’s a healthy cell.
Can cervical cancer be cured completely?
Yes. It’s a highly treatable cancer, especially if it’s caught in the early stages. Healthcare providers typically use the term “remission” to describe a cancer that has gone away. But it can still come back.
Do you need chemo for Stage I cervical cancer?
No. You may not need chemotherapy for Stage I cervical cancer. Surgery is usually the first treatment your provider will recommend for Stage 1. But there are times when chemotherapy is also an option.
Is cervical cancer curable at Stage IV?
A cure at this stage is unlikely, but remission is possible. Stage IV is the most advanced stage of cervical cancer. It means the cancer cells have spread to other organs and tissues throughout your body. Your healthcare provider will still recommend the best ways to try to eliminate the cancer. Radiation therapy, chemotherapy and targeted treatment are still options for you.
Prevention
Can cervical cancer be prevented?
There are some things you can do to help prevent cervical cancer. Receiving regular gynecological exams and getting Pap tests are the most important steps to take toward preventing cervical cancer. Other things you can do are:
- Get the HPV vaccine (if you’re eligible).
- Use condoms or other barrier methods when you have sex.
- Limit your sexual partners.
- Stop smoking and using tobacco products.
Outlook / Prognosis
What’s the outlook for cervical cancer?
Cervical cancer is serious, but it’s highly treatable, especially in the early stages. If you do receive a diagnosis, it’s normal to worry about your health or feel angry that cancer happened to you. You want the cancer to go away so you can continue living a long and fulfilling life. Ask your healthcare provider about what treatment they recommend.
Cancer treatment can be difficult and cause unpleasant side effects. Lean on your loved ones for help. Support groups for people with cancer can also be helpful when you need someone to understand what you’re going through.
Once treatment is over, your healthcare provider will want to monitor you closely to ensure the cancer doesn’t come back. Even if you reach remission, you’ll likely always have cancer in the back of your brain, feeling worried that it can come back. This is a normal response to having cancer. Talking through your feelings with a counselor, close friend or healthcare provider can be beneficial.
What are the survival rates for cervical cancer?
Survival rates for cervical cancer are very good, especially when your provider catches cells at the precancer level (before they change to cancer cells). According to the National Cancer Institute, the five-year relative survival rates are:
- If cervical cancer hasn’t spread, the five-year relative survival rate is 91%. Almost half of all cervical cancers are diagnosed at this stage.
- If cervical cancer has spread outside your cervix to nearby tissues, the five-year relative survival rate is 60%.
- If cervical cancer has spread to your lymph nodes and distant organs, the five-year relative survival rate is about 19%.
These statistics don’t necessarily predict what will happen to you. Your healthcare provider is the best person to discuss your outlook which is unique to you.
Living With
When should I see my healthcare provider?
You should contact a healthcare provider if you notice anything that’s not normal for you. Some things to watch for include:
- Bleeding between menstrual periods or after menopause.
- Watery vaginal discharge.
- Pelvic pain or pain during sex.
Contact your healthcare provider if you’re unsure when your last Pap test was. They can get you on a regular schedule to ensure any changes to your cervix are caught early.
A note from Cleveland Clinic
Receiving a cervical cancer diagnosis can cause a flood of emotions. You’ll likely have many questions over the next several weeks and months. What treatment gives me the best chance at remission? Is the cancer going to come back? Discuss your questions and concerns with your healthcare team to make sure you understand your diagnosis and treatment plan. Treatment could involve surgery, chemotherapy, radiation or a combination of treatments.
It’s easy to put off Pap tests and other gynecological exams. But these tests are critical in detecting cervical cancer early — when it’s most treatable. If you’re unsure when your last Pap test was, talk to a healthcare provider so they can get you on a regular schedule.