Book Appoinment
Prostate Cancer
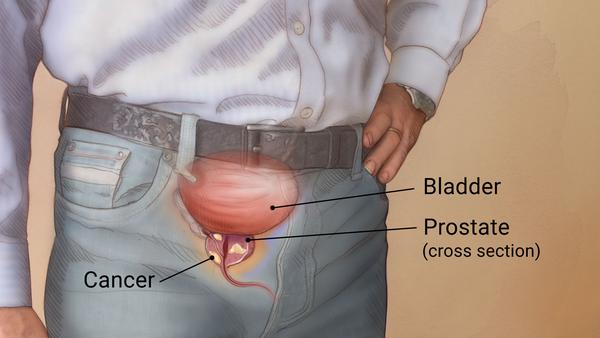
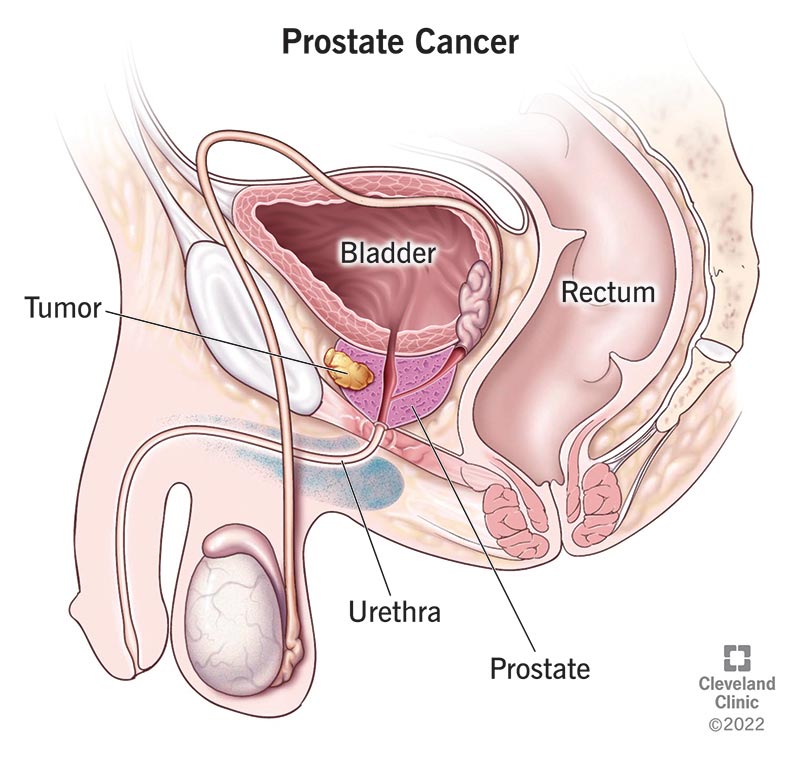
Prostate cancer originates in the prostate gland, which is an essential component of the reproductive system in men and individuals assigned male at birth. This type of cancer often develops slowly and remains confined to the prostate gland for extended periods, leading many patients to opt for active surveillance, where no immediate treatment is administered. This approach allows for careful monitoring of the cancer’s progression. However, in cases where prostate cancer is aggressive and exhibits rapid growth or spreads beyond the prostate, more proactive treatments are necessary. Common treatments for such cases include radiation therapy and surgical interventions, aimed at targeting and managing the cancer effectively.
What causes prostate cancer?
The exact cause of prostate cancer remains uncertain, as experts have not yet pinpointed a specific reason for why prostate cells become cancerous. Like many other cancers, prostate cancer arises when cells in the prostate gland begin to divide more rapidly than normal. In healthy conditions, cells undergo a natural cycle of death and replacement, but cancer cells evade this process. Instead of dying off, these cells continue to multiply uncontrollably, forming a mass known as a tumor. As the tumor grows, parts of it can break away and spread to other areas of the body. Fortunately, prostate cancer generally progresses slowly. Most tumors are detected before they have a chance to spread beyond the prostate, making the cancer highly treatable at this early stage.
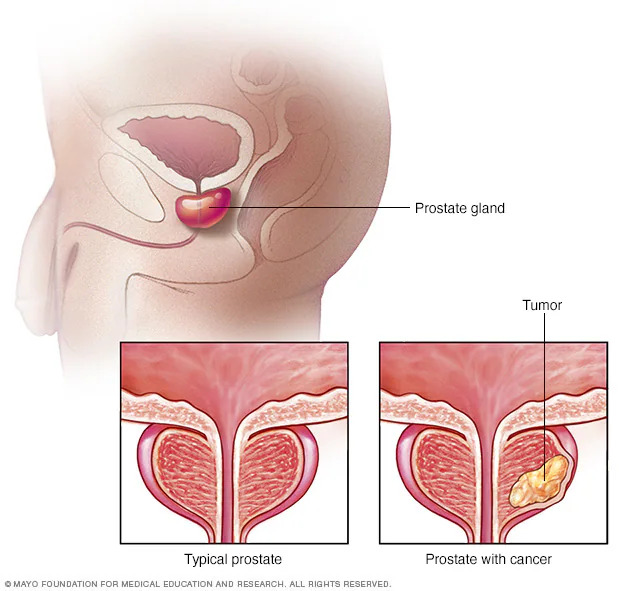
Prostate cancer is a type of cancer that develops in the prostate, a small, walnut-shaped gland in males responsible for producing seminal fluid, which nourishes and transports sperm.
Prostate cancer is among the most prevalent types of cancer, affecting a significant number of men. Often, prostate cancers develop slowly and remain confined to the prostate gland, posing little immediate threat to health. In many cases, these slow-growing cancers may not require extensive treatment and may cause minimal harm over time. However, not all prostate cancers are the same; some are more aggressive in nature. These aggressive forms can spread rapidly beyond the prostate, necessitating prompt and more intensive treatment.
Symptoms
Prostate cancer may cause no signs or symptoms in its early stages.
Prostate cancer that's more advanced may cause signs and symptoms such as:
- Trouble urinating.
- Decreased force in the stream of urine.
- Blood in the urine.
- Blood in the semen.
- Bone pain.
- Losing weight without trying.
- Erectile dysfunction.
Are prostate problems always a sign of prostate cancer?
Not all growths in your prostate are cancer. Other conditions that cause symptoms similar to prostate cancer include:
- Benign prostatic hyperplasia (BPH): At some point, almost everyone with a prostate will develop benign prostatic hyperplasia (BPH). This condition enlarges your prostate gland but doesn’t increase your cancer risk.
- Prostatitis: If you’re younger than 50, an enlarged prostate gland is most likely prostatitis. Prostatitis is a benign condition that causes inflammation and swelling in your prostate gland. Bacterial infections are often the cause.
What causes prostate cancer?
Experts aren’t sure what causes cells in your prostate to become cancer cells. As with cancer in general, prostate cancer forms when cells divide faster than usual. While normal cells eventually die, cancer cells don’t. Instead, they multiply and grow into a lump called a tumor. As the cells continue to multiply, parts of the tumor can break off and spread to other parts of your body (metastasize).
Luckily, prostate cancer usually grows slowly. Most tumors are diagnosed before the cancer has spread beyond your prostate. Prostate cancer is highly treatable at this stage.
What are the risk factors for prostate cancer?
The most common risk factors include:
- Age. Your risk increases as you get older. You’re more likely to get diagnosed if you’re over 50. About 60% of prostate cancers occur in people older than 65.
- Race and ethnicity. You’re at greater risk if you’re Black or of African ancestry. You’re more likely to develop prostate cancers that are more likely to spread. You’re also at greater risk of prostate cancer forming before age 50.
- Family history of prostate cancer. You’re two to three times more likely to get prostate cancer if a close family member has it.
- Genetics. You’re at greater risk if you have Lynch syndrome or if you inherited mutated (changed) genes associated with increased breast cancer risk (BRCA1 and BRCA2).
Some studies have identified other prostate cancer risk factors, but the evidence is mixed. Other potential risk factors include:
- Smoking.
- Prostatitis.
- Having a BMI > 30 (having obesity).
- Sexually transmitted infections (STIs).
- Exposure to Agent Orange (a chemical used during the Vietnam War).
Diagnosis and Tests
How is prostate cancer diagnosed?
Screenings can help catch prostate cancer early. If you’re average risk, you’ll probably have your first screening test at age 55. You may need earlier screenings if you’re in a high-risk group. Screenings usually stop after age 70.
You may need additional tests or procedures if screenings show you may have prostate cancer.
Screening tests for prostate cancer
Screening tests can show whether you have signs of prostate cancer that require more testing:
- Digital rectal exam: Your provider inserts a gloved, lubricated finger into your rectum and feels your prostate gland. Bumps or hard areas may mean cancer.
- Prostate-specific antigen (PSA) blood test: The prostate gland makes a protein called prostate-specific antigen (PSA). High PSA levels may indicate cancer. Levels also rise if you have benign conditions, such as BPH or prostatitis.
Diagnostic procedures for prostate cancer
Not everyone who likely has prostate cancer will need a definitive diagnosis. For example, if your provider thinks your tumor is growing slowly, they may delay more testing because it’s not serious enough to require treatment. If it’s more aggressive (growing fast or spreading), you may need additional tests, including a biopsy.- Imaging: An MRI or a transrectal ultrasound can show images of your prostate gland, including suspicious areas that may be cancer. Imaging results can help your provider decide whether to perform a biopsy.
- Biopsy: During a needle biopsy, a healthcare provider removes a tissue sample for testing in a lab for cancer. A biopsy is the only sure way to diagnose prostate cancer or know for certain how aggressive it is. Your provider may perform genetic tests on the biopsied tissue. Some cancer cells have characteristics (like mutations) that make them more likely to respond to specific treatments.
What are the grades and stages of prostate cancer?
Healthcare providers use the Gleason score and cancer staging to determine how serious the cancer is and the types of treatments you need.
Gleason score
The Gleason score allows your provider to rate how abnormal your cancer cells are. The more abnormal cells you have, the higher your Gleason score. The Gleason score allows your provider to determine the grade of your cancer, or its potential to be aggressive.
Staging prostate cancer
Cancer staging allows your provider to determine how advanced your cancer is, or how much it’s spread. Cancer may be in your prostate gland only (local), invading nearby structures (regional) or spread to other organs (metastasized). Prostate cancer most commonly spreads to your bones and lymph nodes. It can also develop in your liver, brain, lungs and other organs.
Management and Treatment
How is prostate cancer managed or treated?
Your treatment depends on multiple factors, including your overall condition, if the cancer’s spread and how fast it’s spreading. Depending on your treatments, you may work with various healthcare providers, including urologists, radiation oncologists and medical oncologists. Most prostate cancer diagnosed in the early stages can be cured with treatment.
Specific procedures used
Surveillance
Your healthcare provider may monitor your condition instead of providing treatment if your cancer grows slowly and doesn’t spread.
- Active surveillance: You get screenings, scans, and biopsies every one to three years to monitor cancer growth. Active surveillance works best if the cancer grows slowly, is only in your prostate, and isn’t causing symptoms. If your condition worsens, your provider can start treatments.
- Watchful waiting: Watchful waiting is similar to active surveillance, but it’s more commonly used for people who are frailer with cancer that likely won’t go away with treatment. Also, testing is much less frequent. Instead of eliminating the tumor, treatments usually focus on managing symptoms.
Surgery
A radical prostatectomy removes a diseased prostate gland. It can often successfully eliminate prostate cancers that haven’t spread. Your provider can recommend the best removal method if they believe you’d benefit from this surgery.
- Open radical prostatectomy: Your provider makes a single cut (incision) into your abdomen — from your belly button to your pubic bone — and removes your prostate gland. This technique isn’t as common as less-invasive methods like robotic prostatectomy.
- Robotic radical prostatectomy: Robotic radical prostatectomy allows your provider to perform surgery through several tiny incisions. Instead of operating directly, they operate a robot system via a console.
Radiation therapy
You may receive radiation therapy as a standalone treatment for prostate cancer or in combination with other treatments. Radiation can also provide symptom relief.
- Brachytherapy: A form of internal radiation therapy, brachytherapy involves placing radioactive seeds inside your prostate. This approach kills cancer cells while preserving surrounding healthy tissue.
- External beam radiation therapy: With external beam radiation therapy (EBRT), a machine delivers strong X-ray beams directly to the tumor. Specialized forms of EBRT, like IMRT, can direct high doses of radiation toward the tumor while sparing healthy tissue.
Systemic therapies
Your provider may recommend systemic therapies if cancer has spread outside your prostate gland. Systemic therapies send substances throughout your body to destroy cancer cells or prevent their growth.
- Hormone therapy: The hormone testosterone boosts cancer cell growth. Hormone therapy uses medications to combat testosterone’s role in fueling cancer cell growth. The medicines work by preventing testosterone from reaching cancer cells or by reducing your testosterone levels. Alternatively, your provider may recommend surgery to remove your testicles (orchiectomy) so they can no longer make testosterone. This surgery is an option for people who don’t want to take medications.
- Chemotherapy: Chemotherapy uses medicines to destroy cancer cells. You may receive chemotherapy alone or with hormone therapy if your cancer has spread beyond your prostate.
- Immunotherapy: Immunotherapy strengthens your immune system so it’s better able to identify and fight cancer cells. Your healthcare provider may recommend immunotherapy to treat advanced cancer or recurrent cancer (cancer that goes away but then returns).
- Targeted therapy: Targeted therapy zeroes in on the genetic changes (mutations) that turn healthy cells into cancer cells to prevent them from growing and multiplying. Targeted therapies that treat prostate cancer destroy cancer cells with BRCA gene mutations.
Focal therapy
Focal therapy is a newer form of treatment that destroys tumors inside your prostate. Your healthcare provider may recommend this treatment if the cancer is low-risk and hasn’t spread. Many of these treatments are still considered experimental.
- High-intensity focused ultrasound (HIFU): High-intensity sound waves generate powerful heat to kill cancer cells within your prostate.
- Cryotherapy: Cold gases freeze cancer cells in your prostate, eliminating the tumor.
- Laser ablation: Intense heat directed at the tumor kills cancer cells within your prostate, destroying the tumor.
- Photodynamic therapy: Medications make cancer cells more sensitive to certain wavelengths of light. A healthcare provider exposes cancer cells to these light wavelengths, killing the cancer cells.
What are the side effects of prostate cancer treatment?
Potential side effects include:
- Incontinence: You may leak urine when you cough or laugh or feel an urgent need to pee even when your bladder isn’t full. This problem usually improves over the first six to 12 months without treatment.
- Erectile dysfunction (ED): Surgery, radiation and other treatments can damage the erectile nerves in your penis and affect your ability to get or maintain an erection. It’s common to regain erectile function within a year or two (sometimes sooner). In the meantime, medications like sildenafil (Viagra®) or tadalafil (Cialis®) can help by increasing blood flow to your penis.
- Infertility: Treatments can affect your ability to produce or ejaculate sperm, resulting in infertility. If you want children in the future, you can preserve sperm in a sperm bank before starting treatment. After treatments, you may undergo sperm extraction. This procedure involves removing sperm directly from testicular tissue and implanting it into your partner’s uterus.
Talk to your healthcare provider if you’re experiencing treatment side effects. Often, they can recommend medicines and procedures that can help.
Prevention
How can I prevent prostate cancer?
Preventing prostate cancer isn’t possible. Still, taking these steps may reduce your risk:
- Get regular prostate screenings. Ask your healthcare provider how often you should get screened based on your risk factors.
- Maintain a healthy weight. Ask your provider what a healthy weight means for you.
- Exercise regularly. The CDC recommends 150 minutes of moderate-intensity exercise each week, or a little more than 20 minutes daily.
- Eat a nutritious diet. There’s no one diet to prevent cancer, but good eating habits can improve your overall health. Eat fruits, vegetables and whole grains. Avoid red meats and processed foods.
- Quit smoking. Avoid tobacco products. If you smoke, work with your provider on a smoking cessation program to kick the habit.
Outlook / Prognosis
What is the prognosis (outlook) for people with prostate cancer?
Your outlook is excellent if your healthcare provider detects prostate cancer early. Almost everyone — 99% — diagnosed with cancer that hasn’t spread outside of their prostate live at least five years after diagnosis.
Prostate cancer survival rates aren’t as good when the cancer’s metastasized, or spread outside of your prostate. Thirty-two percent of people with metastatic prostate cancer are alive five years later.
Is prostate cancer very curable?
Yes, if it’s caught early. In some cases, cancer grows so slowly that you may not need treatment right away. Treatment can often eliminate prostate cancers that haven’t spread beyond the prostate gland.
When should I call my healthcare provider?
When should I call my healthcare provider?
You should call your healthcare provider if you experience:
- Difficulty peeing.
- Peeing frequently (incontinence).
- Pain when you pee or have intercourse.
- Blood in your pee or semen.
What questions should I ask my healthcare provider?
If you have prostate cancer, you may want to ask your healthcare provider:
- Has the cancer spread outside of my prostate gland?
- What’s the best treatment for the stage of prostate cancer I have?
- What are the treatment risks and side effects?
- Is my family at risk for developing prostate cancer? If so, should we get genetic tests?
- What kind of follow-up care do I need after treatment?
- Should I look out for signs of complications?