Book Appoinment
Colon Cancer
Colon cancer develops from polyps (growths) in your colon’s inner lining. Healthcare providers have screening tests and treatments that detect and remove precancerous polyps. If untreated, colon cancer may spread to other areas of your body. Thanks to these tests, early treatment and new kinds of treatment, fewer people are dying from colon cancer.
What is colon cancer?
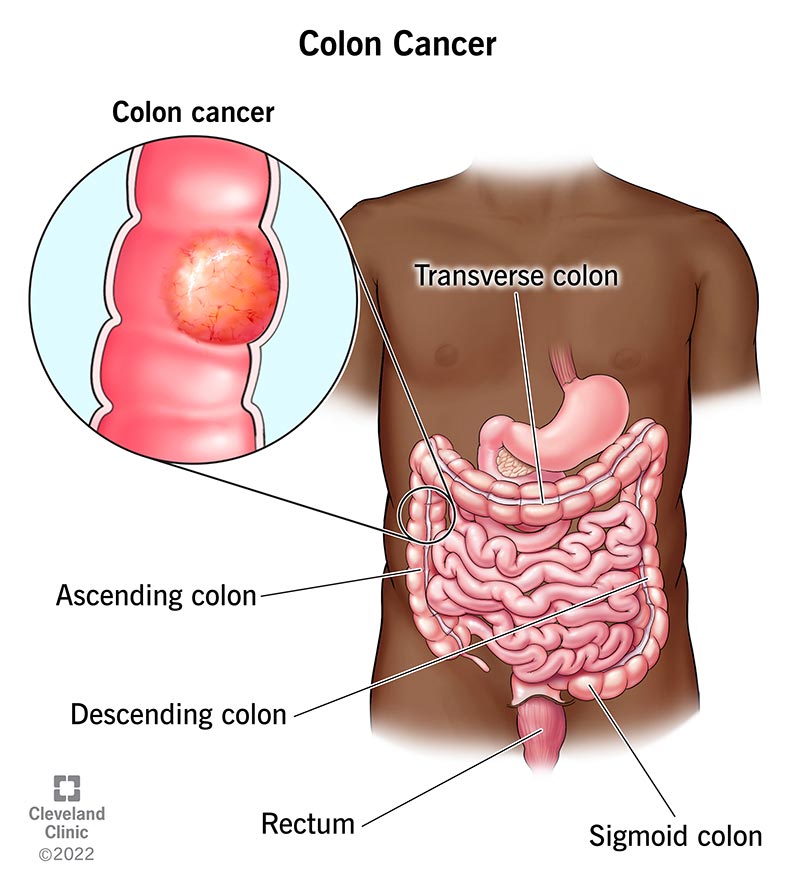
Colon (colorectal) cancer starts in your colon (large intestine), the long tube that helps carry digested food to your rectum and out of your body.
Colon cancer, also known as colorectal cancer, originates in the colon or rectum, which are parts of the large intestine. This type of cancer often begins as benign polyps or abnormal growths in the inner lining of the colon. While these polyps are initially non-cancerous, over time, some may transform into malignant tumors if left unchecked. The development of colon cancer is a gradual process, often taking several years, which provides a critical window for early detection and prevention.
Healthcare providers emphasize the importance of regular screening tests, such as colonoscopies, which are highly effective in identifying and removing precancerous polyps before they have the chance to become cancerous.
How does this condition affect people?
Your colon wall is made of layers of mucous membrane, tissue and muscle. Colon cancer starts in your mucosa, the innermost lining of your colon. It consists of cells that make and release mucus and other fluids. If these cells mutate or change, they may create a colon polyp.
Over time, colon polyps may become cancerous. (It usually takes about 10 years for cancer to form in a colon polyp.) Left undetected and/or untreated, the cancer works its way through a layer of tissue, muscle and the outer layer of your colon. The colon cancer may also spread to other parts of your body via your lymph nodes or your blood vessels.
Who is affected by colon cancer?
Colon cancer is the third most common cancer diagnosed in people in the U.S. According to the U.S. Centers for Disease Control and Prevention (CDC), men and people assigned male at birth (AMAB) are slightly more likely to develop colon cancer than women and people assigned female at birth (AFAB). Colon cancer affects more people who are Black than people who are members of other ethnic groups or races.
Colon cancer, traditionally considered a disease that primarily affects older adults, especially those aged 50 and above, is increasingly being diagnosed in younger populations. Over the past 15 years, the number of individuals aged 20 to 49 diagnosed with colon cancer has risen by approximately 1.5% each year. This trend is concerning to medical professionals and researchers, as it challenges the long-held belief that colon cancer is a disease predominantly affecting older adults.
By staying informed and proactive, individuals can better protect themselves and contribute to the broader effort to combat colon cancer across all age groups.
Symptoms and Causes
What are colon cancer symptoms?
You can have colon cancer without having symptoms. If you do have symptoms, you may not be sure if changes in your body are signs of colon cancer. That’s because some colon cancer symptoms are similar to symptoms of less serious conditions. Common symptoms of colon cancer include:
- Blood on or in your stool (poop): Talk to a healthcare provider if you notice blood in the toilet after you poop or after wiping, or if your poop looks dark or bright red. It’s important to remember blood in poop doesn’t mean you have colon cancer. Other things — from hemorrhoids to anal tears to eating beets — may change your poop’s appearance. But it’s always better to check with a healthcare provider any time you notice blood in or on your stool.
- Persistent changes in your bowel habits (how you poop): Talk to a healthcare provider if you have persistent constipation and/or diarrhea, or if you feel as if you still need to poop after going to the bathroom.
- Abdominal (belly) pain: Talk to a healthcare provider if you have belly pain with no known cause, that doesn’t go away or hurts a lot. Many things may cause belly pain, but it’s always best to check with a healthcare provider if you have unusual or frequent belly pain.
- Bloated stomach: Like belly pain, there are many things that may make you feel bloated. Talk to a healthcare provider if your bloated belly lasts for more than a week, gets worse or you have other symptoms like vomiting or blood in or on your poop.
- Unexplained weight loss: This is a noticeable drop in your body weight when you’re not trying to lose weight.
- Vomiting: alk to a healthcare provider if you’ve been vomiting periodically for no known reason or if you vomit a lot in 24 hours.
- Fatigue and feeling short of breath: These are symptoms of anemia. Anemia may be a sign of colon cancer.
What causes colon cancer?
Like all types of cancer, colon cancer happens when cells grow and divide uncontrollably. All cells in your body are constantly growing, dividing and dying. That’s how your body remains healthy and working as it should. In colon cancer, cells lining your colon and rectum keep growing and dividing even when they’re supposed to die. These cancerous cells may come from polyps in your colon.
Medical researchers aren’t sure why some people develop precancerous colon polyps that become colon cancer. They do know certain risk factors increase people’s chances of developing precancerous polyps and colon cancer.
Those risk factors include certain medical conditions, including inherited conditions, and lifestyle choices. Having one or more risk factors for colon cancer doesn’t mean you’ll develop the condition. It just means you have increased risk. Understanding risk factors may help you decide if you should talk to a healthcare provider about your risk of developing colon (colorectal) cancer.
Lifestyle choices that are risk factors for colon cancer
- Smoking: Using tobacco products, including chewing tobacco and e-cigarettes, increases your risk of developing colon cancer.
- Excessive alcohol use: In general, men and people AMAB should limit beverages containing alcohol to two servings a day. Women and people AFAB should limit beverages containing alcohol to one serving a day. Even light alcohol use can increase your risk of developing cancer.
- Having obesity: Eating high-fat, high-calorie foods may affect your weight and increase your risk of colon cancer.
- Having a diet that includes lots of red meat and processed meat: Processed meat includes bacon sausage and lunchmeat. Healthcare providers recommend you limit red meat and processed meat to two servings a week.
- Not exercising: Any kind of physical activity may reduce your risk of developing colon cancer.
Medical conditions that increase colon cancer risk
- Inflammatory bowel disease: People who have conditions like chronic ulcerative colitis and Crohn’s colitis, which cause inflammation in their colon lining, may have an increased risk of colon cancer. The risk increases if you have inflammatory bowel disease that lasts more than seven years and affects large parts of your colon.
- Inherited conditions: Certain conditions like Lynch syndrome and familial adenomatous polyposis may increase your risk of developing colon cancer. Colon cancer may happen if you inherit a gene that causes cancer.
- A family history of colon and other kinds of cancer: If a close family member has colon cancer, you may have an increased risk of developing the condition. Close family members include your biological parents, siblings and children. Your risk may be higher if any biological family member developed colon cancer before age 45
- A family history of polyps: If your parent, sibling or child has an advanced polyp, you may have an increased risk of getting colon cancer. An advanced polyp may be a large polyp. Medical pathologists may characterize a polyp as being advanced if they see certain changes in the polyp when they look at it under a microscope that are signs the polyp may contain cancerous cells.
- Many polyps: People with numerous colon polyps — including adenomas, serrated polyps or other types of polyps — often have an increased risk of developing polyps and colon cancer. People may inherit a tendency toward having many colon polyps.
What’s the difference between a screening test and tests that diagnose colon cancer?
A cancer screening test checks for cancer when you don’t have any signs or symptoms of cancer. If your screening test shows abnormalities, a healthcare provider may recommend additional tests
What are common colon cancer screening tests?
A colonoscopy is the most common screening test for colon cancer. Other tests include:
- Fecal immunochemical test (FIT): This test detects hidden blood in your poop. Medical pathologists test samples of your poop for blood that you may not see just by looking.
- Guaiac-based fecal occult blood test (gFOBT): Like the FIT, this test looks for blood in poop that may not be visible.
- Fecal DNA test: This test looks for signs of genetic mutations and blood products in your poop.
- Flexible sigmoidoscopy: Healthcare providers use a flexible scope called a sigmoidoscope to see inside your lower colon and rectum.
- Virtual colonoscopy: A virtual colonoscopy is an X-ray that looks for polyps, tumors and ulcers (sores) in your colon and rectum.
How do healthcare providers stage colon cancer?
Healthcare providers use the TNM cancer staging system developed by the American Joint Committee on Cancer to stage colon cancer.
There are five stages of colon cancer. Three of the four stages have three sub-stages. The colon cancer staging system includes the following:
Stage 0: Healthcare providers may refer to this as carcinoma in situ. When they do, they’re talking about abnormal or precancerous cells in your mucosa, the innermost layer of your colon wall.
Stage I: Stage I colorectal cancer has grown into the wall of your intestine but hasn’t spread beyond the muscular coat or into close lymph nodes.
Stage II:The cancer has spread farther into the wall of your intestine but hasn’t spread to nearby lymph nodes. There are three types of Stage II colon cancer:
- Stage IIA: Cancer has spread through most of your colon wall but hasn’t grown into the wall’s outer layer.
- Stage IIB: Cancer has spread into the outer layer of your colon wall or through the wall.
- Stage IIC: Cancer has spread to a nearby organ.
Stage III: In this stage, colon cancer has spread to your lymph nodes. Like Stage II colon cancer, there are three sub-stages of Stage III colon cancer:
- Stage IIIA: Cancer has spread through most of your colon wall but hasn’t grown into the wall’s outer layer.
- Stage IIIB: The cancer affects more layers of your colon wall but only affects one to three lymph nodes. Cancer that affects fewer colon wall layers but has spread to four or more lymph nodes is also a stage IIIB colon cancer.
- Stage IIIC: There’s cancer in the outer layer or the next outermost layer of your colon and in four or more lymph nodes. Cancer that’s spread into a nearby organ and one or more lymph nodes is also a stage IIIC colon cancer.
Stage IV: Cancer has spread (metastasized) to other areas of your body, such as your liver, lungs or ovaries:
- Stage IVA: In this stage, cancer has spread to one organ or to lymph nodes that are farther or more distant from your colon.
- Stage IVB: Cancer affects distant organs, lymph nodes and abdominal tissue.
Management and Treatment
How do healthcare providers treat colon cancer?
Surgery is the most common colon cancer treatment. There are different colon cancer surgeries and procedures:
- Polypectomy: This surgery removes cancerous polyps.
- Partial colectomy: This is also called colon resection surgery. Surgeons remove the section of your colon that contains a tumor and some surrounding healthy tissue. They’ll reconnect healthy colon sections in a procedure called anastomosis.
- Surgical resection with colostomy: Like a colectomy, surgeons remove the section of your colon that contains a tumor. In this surgery, however, they can’t connect healthy colon sections. Instead, they do a colostomy. In a colostomy, your bowel is moved to an opening in your abdominal wall so your poop is collected in a bag.
- Radiofrequency ablation: This procedure uses heat to destroy cancer cells.
Healthcare providers may combine surgery with adjuvant therapy. This is cancer treatment done before or after surgery. They may also use these treatments for colon cancer that has spread or come back. Treatments may include:
- Chemotherapy: Healthcare providers may use chemotherapy drugs to shrink tumors and ease colon cancer symptoms.
- Targeted therapy: This treatment targets the genes, proteins and tissues that help colon cancer cells grow and multiply. Healthcare providers often use a type of targeted therapy called monoclonal antibody therapy. This therapy uses lab-created antibodies that attach to specific targets on cancer cells or cells that help cancer cells grow. The antibodies kill the cancer cells.
Prevention
Can colon cancer be prevented?
You may not be able to prevent colon cancer, but you can reduce your risk of developing the condition by managing risk factors:
- Avoid tobacco. If you smoke and want help quitting, talk to a healthcare provider about smoking cessation programs.
- Use moderation when you drink beverages containing alcohol.
- Maintain a healthy weight.
- Eat a healthy diet. Add fruit and vegetables to your diet and cut back on red meat processed foods, and high-fat and high-calorie foods. Drinking coffee may lower your risk of developing colon cancer.
- Keep track of your family medical history.Colon cancer can run in families. Tell your healthcare provider if your biological parents, siblings or children have colon cancer or an advanced polyp or if any of your family has cancer before age 45.
- Follow colon cancer screening guidelines.Ask your healthcare provider when you should have colon cancer screening. If you have chronic irritable bowel disease or a family history of colon cancer, your healthcare provider may recommend you start screening earlier than age 45.
Outlook / Prognosis
Can healthcare providers cure colon cancer?
According to U.S. National Cancer Institute (NCI) data, more than 90% of people treated for early-stage colorectal cancer were alive five years after diagnosis. (NCI data doesn’t break out separate survival rates for colon and rectal cancer.)
What are the survival rates for colon cancer?
NCI data shows that overall, 65% of people with colorectal cancer were alive five years after diagnosis. (A survival rate is an estimate based on the experiences of people with specific kinds of cancer.)
Colorectal cancer survival rates vary based on the cancer stage at diagnosis. For example, 73% of people with colorectal cancer that’s spread to nearby tissues, organs or lymph nodes were alive five years after diagnosis. That five-year survival rate drops to 17% if the cancer spreads to a distant organ or lymph node.
A survival rate is an estimate based on outcomes — how long people lived after treatment for a specific type of cancer. In this case, survival rates are based on the experiences of large groups of people who have colorectal cancer, and not just colon cancer. In addition, many things affect colon cancer survival rates. If you have this condition, your healthcare provider is your best resource for information about what you can expect.
Living With
I have colon cancer. How do I take care of myself?
Self-care is an important part of living with colon cancer, but everyone’s situation is different. People treated for early-stage colon cancer may become cancer-free. They’re cancer survivors, but they may worry that their colon cancer will come back.
People who have advanced colon cancer have different concerns. They’re also cancer survivors. But for them, living with colon cancer may mean treatment that eases symptoms but doesn’t cure colon cancer. They may benefit from having palliative care. Palliative care helps people manage cancer symptoms and treatment side effects.
When should I see my healthcare provider?
Follow-up colon cancer care varies depending on the cancer stage. For example, people who have surgery for Stage 0 or Stage I colon cancer may have a colonoscopy one year after surgery, another colonoscopy three years after surgery and a third five years after surgery.
Unless the follow-up colonoscopies find signs of cancer, someone with Stage 0 or Stage 1 colon cancer may be able to wait several more years before having another colonoscopy.
People successfully treated for Stage II or Stage III colon cancer will need to see their healthcare provider every three to six months for the first two years after treatment and are typically followed for five years from surgery. They may have tests including colonoscopies, CEA blood tests and imaging tests.
Anyone recovering from colon cancer treatment should contact their healthcare provider if they notice changes that may indicate the cancer has come back or is spreading.
When should I go to the emergency room?
If you’re receiving colon cancer treatment, ask your healthcare provider about symptoms that may be signs you should go to the emergency room. You may need to go to the emergency room if you have:
- Side effects that are more intense than you expected.
- A fever higher than 100.4 degrees Fahrenheit (38 degrees Celsius).
- Chills that don’t go away.
- Severe abdominal pain.
- Persistent diarrhea that causes dehydration.
What questions should I ask my doctor?
Most people have heard of colon cancer, which is the third most common cancer diagnosed in the U.S. If you have colon cancer, you probably want to know more about your specific situation. Here are some questions you may want to ask your healthcare provider:
- What kind of colon cancer do I have?
- Can you cure this kind of colon cancer?
- What is the cancer stage?
- What are effective colon cancer treatments?
- If I need surgery, what kind of surgery do you recommend?
- Will I need a colostomy?
- Will I need other kinds of cancer treatments?
- What are those treatment side effects?
- Is a clinical trial an option for me?
- What is the chance my colon cancer could come back?
- If you can’t cure the cancer, can you keep it from spreading?
- If you can’t stop the cancer, should I have palliative care?
A note from Cleveland Clinic
Thanks to more people taking time for colon cancer screening, healthcare providers are able to catch and treat colon cancer before it causes symptoms, much less spreads. Recent survival rate data show that more than 90% of people treated for early-stage colon cancer were alive five years after diagnosis. People with colon cancer also benefit from having newer treatments that target cancer. If you have colon cancer, ask your healthcare provider about newer treatments that may be appropriate for your situation.