Book Appoinment

Pancreatic Cancer
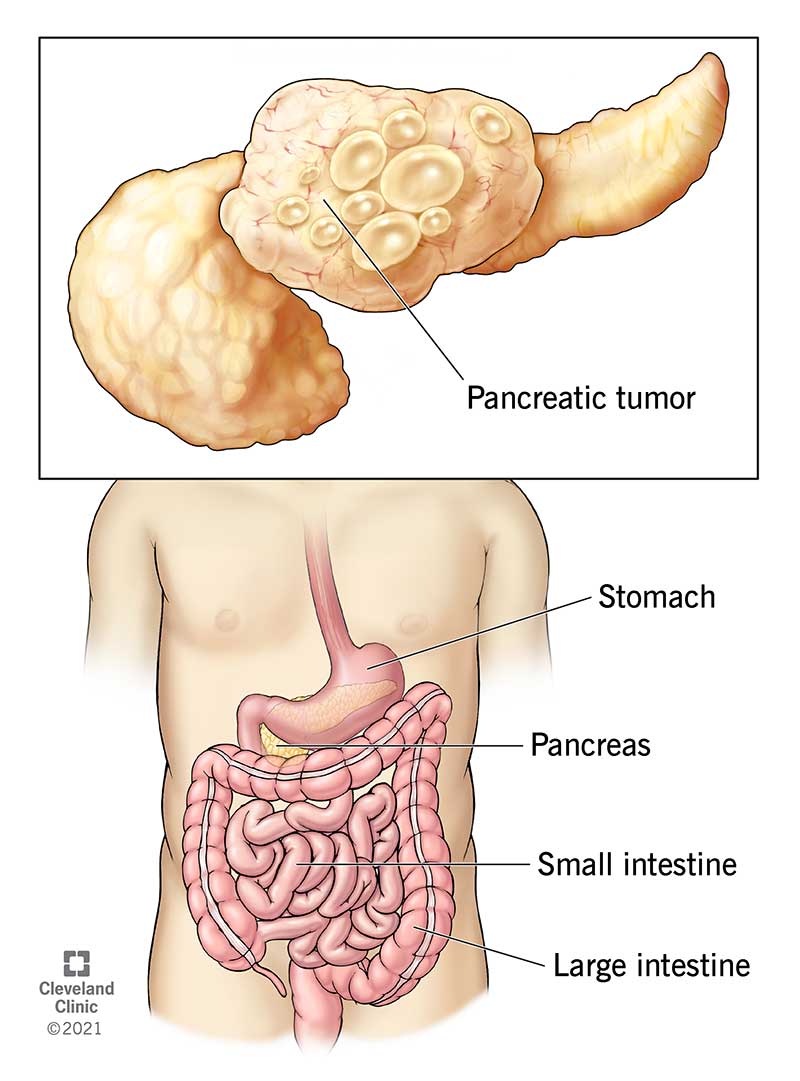
Pancreatic cancer affects your pancreas, a gland in your abdomen that aids in digestion. Pancreatic cancer symptoms include nausea, bloating, fatigue, jaundice and lack of appetite. Treatments include surgery, chemotherapy and radiation therapy. Pancreatic cancer survival rates are low because the disease is difficult to detect in the early stages.
Overview
What is pancreatic cancer?
Pancreatic cancer occurs when cells in your pancreas mutate (change) and multiply out of control, forming a tumor. Your pancreas is a gland in your abdomen (belly), between your spine and stomach. It makes hormones that control blood-sugar levels and enzymes that aid in digestion.
Most pancreatic cancers start in the ducts of your pancreas. The main pancreatic duct (the duct of Wirsung) connects your pancreas to your common bile duct.
Early-stage pancreatic tumors don’t show up on imaging tests. For this reason, many people don’t receive a diagnosis until the cancer has spread (metastasis). Pancreatic cancer is also resistant to many common cancer drugs, making it notoriously difficult to treat.
Ongoing research focuses on early detection through genetic testing and new imaging methods. Still, there’s much to learn.
Types of pancreatic cancer
There are two main types of pancreatic tumors:
- Exocrine tumors: Over 90% of all pancreatic tumors are exocrine tumors. The most common type of pancreatic cancer is adenocarcinoma, which begins in the cells that line your organs.
- Neuroendocrine tumors: Less than 10% of pancreatic tumors are neuroendocrine tumors (NETs). Islet cell carcinoma is another name for an NET.
How common is pancreatic cancer?
Pancreatic cancer is responsible for approximately 3% of all cancers in the United States. It’s the 10th most common cancer in men and people assigned male at birth, and the 8th most common cancer in women and people assigned female at birth.
Cases of pancreatic cancer are on the rise. Trends indicate that pancreatic cancer will be the second leading cause of cancer death in the United States by 2030.
Symptoms and Causes
What are the symptoms of pancreatic cancer?
Unfortunately, there aren’t any early signs of pancreatic cancer. Symptoms typically emerge once the tumor starts impacting other organs in your digestive system.
Pancreatic cancer symptoms may include:
- Jaundice (yellowing of your skin).
- Dark urine (pee).
- Light-colored stool (poop).
- Upper abdominal pain.
- Middle back pain.
- Fatigue.
- Itchy skin.
- Nausea and vomiting.
- Gas or bloating.
- Lack of appetite.
- Blood clots.
- Weight loss.
- New-onset diabetes.
Your healthcare provider might suspect pancreatic cancer if you’ve recently developed diabetes or pancreatitis — a painful condition due to inflammation in your pancreas.
Symptoms of pancreatic neuroendocrine cancer may be different from traditional pancreatic cancer symptoms, such as jaundice or weight loss. Symptoms can vary, but may include diarrhea and anemia.
How long does it take to notice pancreatic cancer?
There are no tell-tale early signs of pancreatic cancer. Some people develop vague symptoms up to one year before they receive a diagnosis.
Many people report that their first pancreatic cancer symptoms were back pain or stomach pain. These symptoms can come and go at first, but may get worse after meals or when you lie down.
What causes pancreatic cancer?
There isn’t a clear answer. We don’t know exactly what causes pancreatic cancer. But experts have identified some risk factors.
Pancreatic cancer risk factors
A risk factor is something that increases your chances of getting a certain disease. Common pancreatic cancer risk factors include:
- Smoking cigarettes, cigars and using other forms of tobacco.
- Obesity, particularly if you carry extra weight around your waist.
- Diabetes, especially Type 2 diabetes. Sudden-onset diabetes could be a sign of pancreatic cancer.
- Exposure to certain chemicals, like pesticides and petrochemicals.
- Chronic pancreatitis, a permanent inflammation of your pancreas.
- Hereditary chronic pancreatitis due to gene changes (mutations) passed from biological parent to child.
- Hereditary syndromes with changes (mutations) in genes, such as BRCA1 or BRCA2 genes passed from biological parent to child.
What are the complications of pancreatic cancer?
Pancreatic cancer tends to spread (metastasize) to nearby blood vessels, lymph nodes, and then to your liver, peritoneum (the lining of your abdominal cavity) and lungs
The majority of pancreatic cancers have already spread beyond the pancreas at the time of diagnosis.
Diagnosis and Tests
How is pancreatic cancer diagnosed?
It’s difficult to detect pancreatic cancer in the early stages. This is because healthcare providers can’t feel your pancreas during routine exams and it’s difficult to see these tumors on routine imaging tests.
If your provider suspects pancreatic cancer, they’ll recommend a combination of pancreas function tests, which may include:
Imaging tests
Your healthcare provider may need to take one or more of the following imaging tests:
- CT (computed tomography) scans.
- MRI (magnetic resonance imaging).
- PET (positron emission tomography).
- Endoscopic ultrasound (EUS).
Blood tests
A pancreas blood test can detect tumor markers. A tumor marker is a substance that may indicate the presence of cancer.
For pancreatic cancer, high levels of carbohydrate antigen (CA) 19-9 — a type of protein released by pancreatic cancer cells — might indicate a tumor.
Staging laparoscopy
Sometimes, providers use laparoscopy to determine the extent of pancreatic cancer and whether removal is possible.
During this procedure, a surgeon creates a few small incisions (cuts) in your abdomen and inserts a long tube with a camera on the end. This allows them to see inside your abdomen and look for abnormalities. Often, they’ll take a biopsy during the same procedure.
Genetic testing
If you receive a pancreatic cancer diagnosis, you should consider genetic testing. This can tell you if there’s a hereditary reason you developed pancreatic cancer. It can also help your healthcare provider determine which type of treatment will be most effective for you.
Some people with pancreatic cancer have mutations in genes BRCA1 and BRCA2. Though you may recognize these genes as the “breast cancer genes,” mutations in BRCA1 and BRCA2 may also indicate other types of cancer, including prostate, ovarian and pancreatic.
If you’re a first-degree relative (a parent, child or sibling) of someone who has pancreatic cancer, you should consider genetic testing. Your results can tell you if you have a BRCA1 or BRCA2 gene mutation. Keep in mind, even if you have the mutation, it doesn’t mean you’ll get cancer. But knowing your risk is important.
Resectable vs. unresectable pancreatic cancer: What’s the difference?
Healthcare providers rank pancreatic tumors into four different categories:
- Resectable: The tumor is only in your pancreas and doesn’t involve nearby blood vessels or other organs. A provider can remove it with surgery.
- Borderline resectable: The tumor is in your pancreas and there’s some involvement of nearby blood vessels, but a surgeon can still remove it.
- Locally advanced: The tumor is in your pancreas and has significant involvement of nearby blood vessels. In these cases, surgical removal might be difficult or unsafe.
- Metastatic: The cancer has spread to distant areas in your body, such as your liver, lungs or abdominal cavity. It has possibly spread to organs, tissues or lymph nodes near your pancreas.
If you have specific questions about pancreatic cancer staging, talk to your healthcare provider. Understanding your pancreatic cancer diagnosis can help you make an informed decision about your treatment.
Management and Treatment
Is pancreatic cancer curable?
Even though pancreatic cancer has a poor survival rate, complete remission is possible with early detection and treatment. The only way to realistically cure pancreatic cancer is total surgical removal of the cancer.
How is pancreatic cancer treated?
Specific treatment depends on certain factors, including:
- The exact location of the tumor.
- What stage it is.
- Your overall health.
- Whether the cancer has spread beyond your pancreas.
Pancreatic cancer treatments include:
Surgery
Surgery is the only realistic way to cure pancreatic cancer. But surgeons only recommend it when they think they can remove all of the cancer. Otherwise, there’s little to no benefit.
For surgery to be successful, the cancer must be completely confined to the pancreas. Even then, total cancer removal may not be possible.
There are a few different surgical techniques, depending on the location and size of the tumor:
Whipple procedure (pancreaticoduodenectomy)
If the tumor is in the head of your pancreas (the widest part of your pancreas, near your small intestine), your provider may recommend the Whipple procedure. This surgical approach removes the head of your pancreas, your duodenum (the first portion of your small intestine), your gallbladder, a portion of your bile duct and nearby lymph nodes.
Your surgeon will then attach your remaining bile duct and pancreas to your small intestine. This reestablishes your digestive tract.
Distal pancreatectomy
If the tumor is in the tail of your pancreas, a surgeon can perform a distal pancreatectomy. During this procedure, a surgeon removes the tail of your pancreas and some of the pancreas body. In most cases, they’ll also remove your spleen.
As your spleen helps fight infections, your healthcare provider may recommend getting certain vaccinations before having a distal pancreatectomy.
Total pancreatectomy
If cancer has spread throughout your entire pancreas, but resection (removal) is still possible, your healthcare provider may consider a total pancreatectomy. This surgery removes your entire pancreas, gallbladder, spleen and part of your stomach and small intestine.
It’s possible to live without a pancreas, but it can cause major side effects. Your pancreas makes insulin and other hormones that keep blood sugar at a safe level. Without a pancreas, you’ll develop diabetes and need insulin shots to survive. Additionally, you’ll need to take pancreatic enzyme pills to help with digestion.
Chemotherapy
Chemotherapy uses drugs that kill cancer cells. Healthcare providers give these drugs in pill form or through an IV in your arm.
Providers use chemotherapy as a stand-alone treatment — especially for people with advanced pancreatic cancer. They may also recommend chemotherapy before surgery to shrink the tumor or after surgery to kill any remaining cancer cells.
Radiation therapy
Radiation therapy uses high-energy X-rays to kill cancer cells. Healthcare providers commonly use this approach to treat pancreatic cancer.
Most often, providers combine radiation therapy with chemotherapy (chemoradiation). They may recommend it before surgery, after surgery or as part of your main cancer treatment. Radiation therapy can also help ease pancreatic cancer symptoms in people who don’t qualify for surgery (in cases of advanced cancer).
Targeted therapy
This treatment uses drugs that “target” certain proteins. These proteins control how cancer cells grow and spread. Providers may combine targeted therapy with other treatments like radiation therapy.
Common targeted therapy drugs for pancreatic cancer include:
- Erlotinib.
- Olaparib.
- Larotrectinib.
- Entrectinib.
Pain management
Pancreatic cancer could be very painful as it may involve nearby nerves. Your healthcare provider can help you manage pain with oral medications, anesthesia or steroid injections.
If you have pancreatic cancer and start to develop severe and persistent pain, tell your healthcare provider. They can find a treatment that will ease your symptoms.
Prevention
Can I prevent pancreatic cancer?
You can’t prevent pancreatic cancer. But there are things you can do to lower your risk:
- Don’t smoke.
- Limit your alcohol intake.
- Eat lots of fresh fruit, vegetables, and whole grains.
- Reduce your intake of red meat, sugary drinks, and processed foods.
- Limit your exposure to harmful chemicals, such as asbestos, pesticides, and petrochemicals.
- Maintain a weight that’s healthy for you.
Pancreatic cancer screenings
Healthcare providers don’t usually perform routine screenings for pancreatic cancer. But in people with a high risk of pancreatic cancer due to genetic predisposition, providers recommend monitoring with imaging tests and endoscopic ultrasounds.
If you have a first-degree family member (parents or siblings) with pancreatic cancer, you should talk to a healthcare provider about your risk of developing pancreatic cancer and proper screening and genetic tests.
Outlook / Prognosis
What can I expect if I have pancreatic cancer?
A pancreatic cancer diagnosis can feel overwhelming. Because everyone is unique, no two cases are the same. Your healthcare provider will assemble a team of experts to determine the best treatment plan for your situation. Your medical team may include:
- Gastroenterologist.
- Pathologist.
- Oncologists (medical, surgical, and radiation).
- Social worker.
Pancreatic cancer progression timeline
Generally, it takes about 10 to 20 years for a single cancer cell in your pancreas to turn into a tumor. The goal of ongoing research is to determine how healthcare providers can detect pancreatic cancer in its earliest stages, when it’s more treatable.
Pancreatic cancer survival rate
In the United States, the five-year survival rate for people with pancreatic cancer is 11%. This means that 11 out of 100 people are still alive five years after their diagnosis.
Survival rates are only estimates. They can’t tell you how long you’ll live or how well you’ll respond to treatment. If you have specific questions about survival rates and what they mean for you, talk to your healthcare provider.
Living With
When should I see my healthcare provider?
There are no clear-cut symptoms for early-stage pancreatic cancer. However, you should see a healthcare provider right away if you develop:
- Jaundice.
- Stomach or back pain.
- Unexplained weight loss.
- Sudden onset of diabetes.
What questions should I ask my healthcare provider?
Develop an open and cooperative relationship with your healthcare provider. If you or a loved one received a pancreatic cancer diagnosis, here are some questions you may want to ask:
- What stage is the cancer? What does this mean for me?
- What are my treatment options? Which do you recommend and why?
- What side effects might I develop as a result of treatment?
- Is genetic testing right for me?
- Are there clinical trials available?
- Will I be able to keep working and doing the things that I need to do every day?
- Can you tell me where to find financial support?
- Can you tell me where to find emotional support?
- What should I do to stay as healthy as I can?
Additional Common Questions
What are some signs that pancreatic cancer has spread?
As pancreatic cancer progresses, you may develop new symptoms. Advanced pancreatic cancer symptoms may include:
- Abdominal pain.
- Extreme fatigue.
- Unexplained weight loss.
- Jaundice.
- Fluid buildup and swelling in your abdomen (ascites).