Book Appoinment
Thrombosis
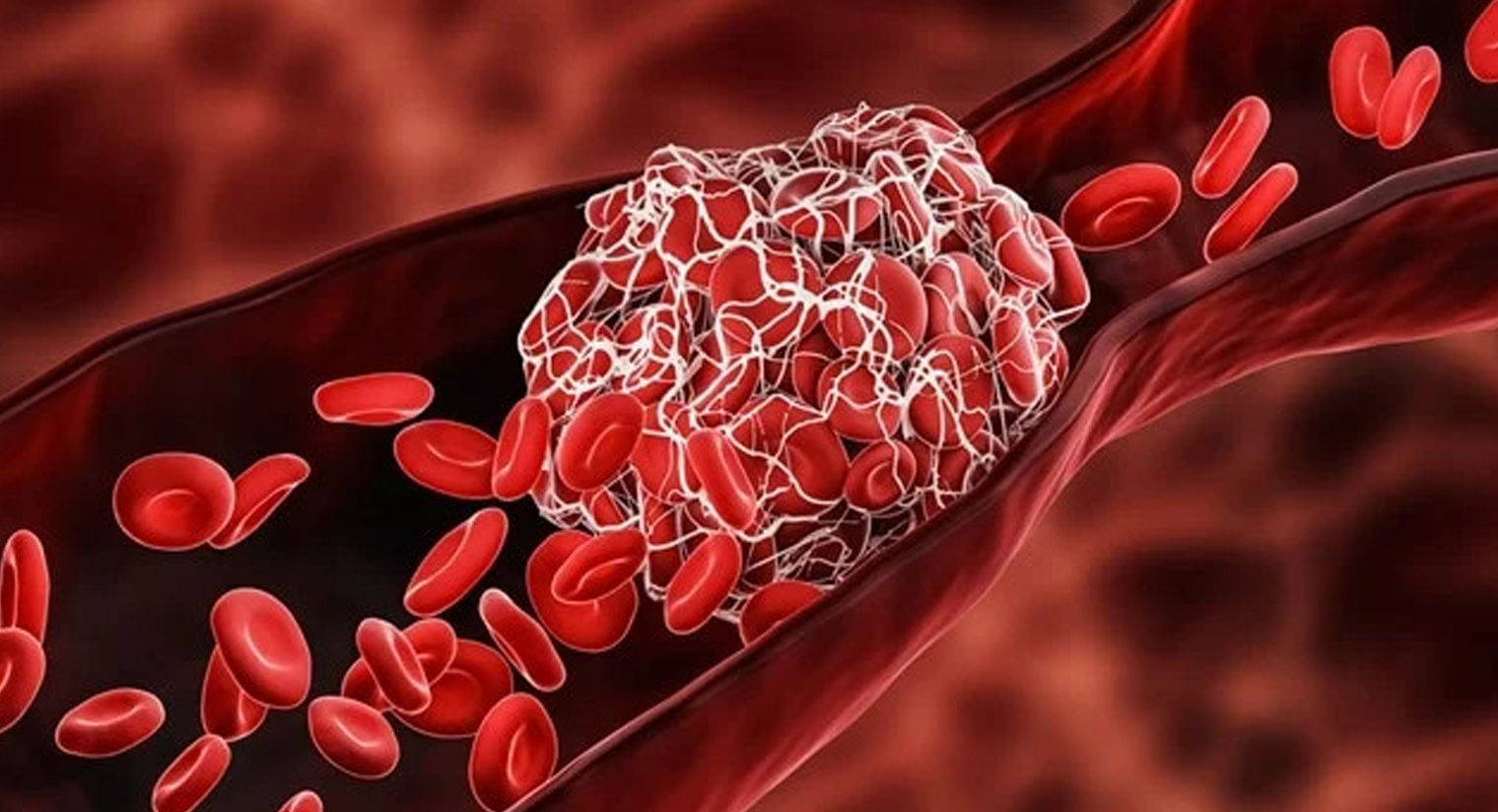
Thrombosis is a serious condition where one or more blood clots form in your blood vessels or heart. When this happens, the clot can block blood flow where it formed, or it can break loose and travel elsewhere in your body. If a moving clot gets stuck in a critical area, it can cause life-threatening conditions like stroke and heart attack.
Overview
What is thrombosis?
Thrombosis is the formation of a blood clot (thrombus) inside one of your blood vessels or a chamber of your heart. Clots can block blood flow in your blood vessels or break free and travel elsewhere in your body. If a clot gets stuck in a critical location like your lungs or brain, it can disrupt blood flow to that organ and result in a life-threatening emergency. Symptoms vary based on the clot’s location and can include chest pain, trouble breathing and skin changes.
Some people face a higher risk of thrombosis due to medical conditions or other factors. Learning your risk can help you prevent thrombosis, and learning the symptoms can help you recognize problems if they occur.
Thrombosis is a serious condition, and it can become more dangerous as time passes. It can quickly turn into a medical emergency. The sooner you seek care for thrombosis, the better your chances of a good outcome.
If you or someone with you has symptoms of thrombosis, seek emergency medical care immediately.
Complications of thrombosis
Thrombosis can lead to many different complications depending on where the blood clot forms or travels to:
- Lungs: Pulmonary embolism.
- Brain: Transient ischemic attack (TIA) or stroke.
- Heart (coronary artery): Heart attack.
- Neck (carotid artery): TIA or stroke.
- Belly (superior mesenteric artery or one of its branches): Mesenteric ischemia.
Types of thrombosis
The two main types of thrombosis are:
- Arterial thrombosis: This is when a blood clot forms in an artery. Your arteries carry blood from your heart to the rest of your body. Arterial thrombosis is the most common cause of heart attacks and strokes.
- Venous thrombosis: This is when a blood clot forms in a vein. Veins carry blood back to your heart from your body. Venous thrombosis is the most common cause of a pulmonary embolism (blood clot in your lung).
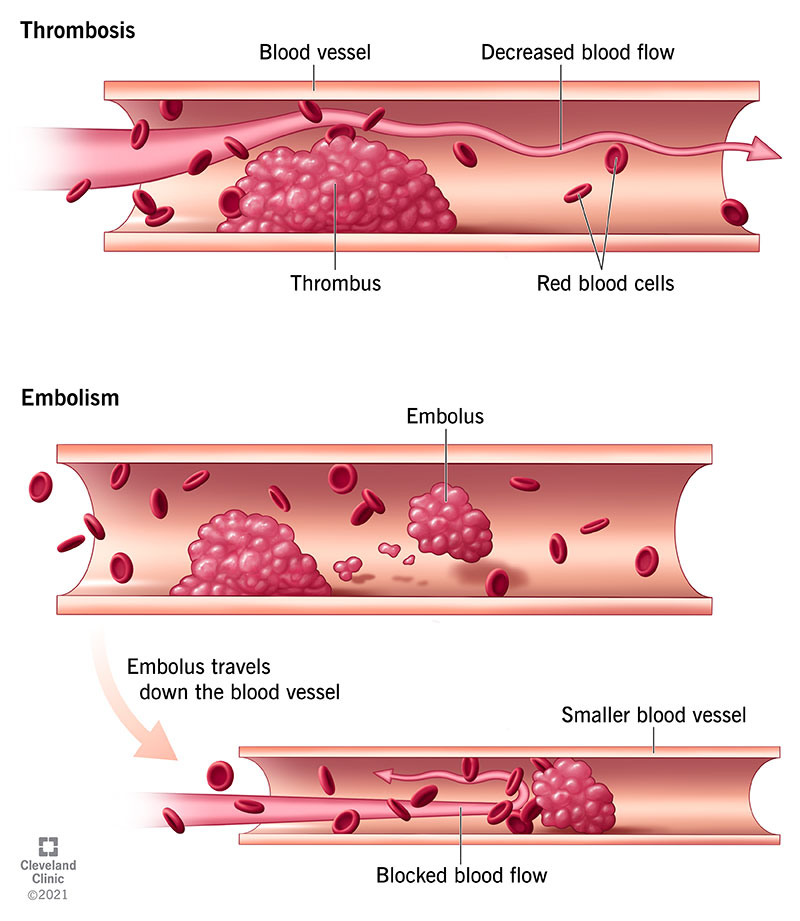
Thrombosis is dangerous in either location (artery or vein) because it can:
- Cause a blockage where it forms: The clot may stay in place and grow until it’s big enough to block blood flow. The severity of that blockage depends on where the clot forms and how big it grows.
- Cause a blockage somewhere else: The clot may break free from its origin and become an embolus. It can then travel in your blood and get stuck in a smaller blood vessel, creating a blockage (embolism). This is usually what causes conditions like stroke and pulmonary embolism.
How common is thrombosis?
Thrombosis is extremely common and is the underlying cause of 1 in 4 deaths worldwide. That’s because thrombosis can lead to dangerous conditions like a heart attack, stroke or pulmonary embolism.
Thrombosis is more common among people with certain medical conditions, including:
- Atrial fibrillation.
- Cancer.
- Coronary artery disease.
- Diabetes.
- Clotting disorders such as antiphospholipid syndrome.
- Tobacco use.
Symptoms and Causes
What are the symptoms of thrombosis?
Thrombosis symptoms depend on the size of the clot, its location (where it forms or gets stuck) and the complications it causes. Blockages are more likely to occur in areas with very small blood vessels, especially your lungs, brain and farther down in your legs and arms. Listed below are common symptoms for each location:
Lungs (pulmonary embolism)
- Sharp pain in your chest and surrounding areas (jaw, neck, shoulder, back, or arm).
- Pain when you breathe in.
- Sudden trouble breathing when active or at rest.
Brain or neck (transient ischemic attack (TIA) or stroke)
- Weakness or trouble controlling muscles on one side of your body.
- Slurred or garbled speech.
- Noticeable droop and lack of muscle control on one side of your face.
- Confusion, agitation, or otherwise unusual behavior changes.
Heart (heart attack)
- Chest pain or discomfort (angina).
- Trouble breathing.
- Dizziness or passing out.
- People assigned female at birth often have additional symptoms.
Belly (mesenteric ischemia)
- Severe stomach or abdominal pain, especially after eating.
- Bloating, nausea, and vomiting.
- Diarrhea, which may contain blood.
- Fever.
Artery in arm or leg
- Skin that looks paler than other areas.
- Skin that feels cool to the touch.
- Weakness and inability to move the affected body part.
- Numbness or tingling (pins and needles), possibly with pain.
- Blisters, wounds, or sores.
- Skin sloughing, which is when skin falls away from the tissue underneath.
- Necrosis, or tissue death.
Vein in arm or leg
- Skin that looks redder or darker than other areas.
- Pain, especially around the affected area.
- Swelling from fluid buildup.
- Skin that feels warm to the touch.
What causes thrombosis?
Thrombosis happens when something damages the inner lining of your blood vessel (endothelium) or slows blood flow. In either case, cells in your blood start to stick together when they shouldn’t.
Normally, many cells in your blood coexist in harmony and come together when needed for a certain job. For example, if you have a wound, platelets and proteins join together at the site of injury to serve as a plug. This multistage process (hemostasis) forms a necessary clot that stops you from losing too much blood. The clot dissolves when your wound heals. It’s like an emergency meeting at work when everyone huddles at one desk. When the problem’s solved, everyone leaves and goes their separate ways.
But various medical conditions, medications and other factors can cause components of your blood to cluster together when they don’t need to or fail to dissolve when they should. As a result, a blood clot (thrombus) may form from clumps of blood clotting components and potentially get bigger. It may also break away and travel through your bloodstream until it gets stuck in a smaller blood vessel (embolus).
Both of these situations can lead to dangerous — or even life-threatening — complications. That’s why it’s important to learn what may put you at risk.
What are the risk factors?
Anything that interferes with your blood’s ability to flow freely or clot normally can raise your risk for thrombosis. This includes many conditions, medications and lifestyle factors.
Specific risk factors include:
- Atherosclerosis.
- Atrial fibrillation.
- Being over age 60.
- Blood clotting disorders.
- Cancer.
- Chemotherapy.
- Diabetes.
- Family history of blood clots.
- Having certain surgeries or procedures, including central line placement.
- Heart failure.
- Heart valve disease.
- High blood pressure.
- High cholesterol.
- Inflammatory or autoimmune diseases.
- Obesity.
- Paralysis of a leg.
- Pregnancy.
- Prior heart attack or stroke.
- Sitting still for too long for various reasons, including long flights or bed rest.
- Tobacco use.
- Using birth control pills containing estrogen.
- Using hormone replacement for menopause symptoms.
Diagnosis and Tests
How is thrombosis diagnosed?
Healthcare providers diagnose thrombosis based on:
- A physical exam.
- Imaging tests.
- Blood tests.
Physical exam
During a physical exam, a provider will:
- Ask you questions about your symptoms and medical history.
- Look at different areas of your body for visible signs of thrombosis.
- Feel areas of concern to check for swelling, tissue changes, or temperature changes.
- Use a stethoscope to listen to your heart, breathing, and digestive system.
- Check the pulses in your arms or legs.
Imaging tests
Imaging tests let your provider see inside your body. Possible tests you may need include:
- Computed tomography (CT) scans.
- Magnetic resonance imaging (MRI).
- Ultrasound.
- X-rays of your blood vessels (angiogram or venogram).
Blood tests
Blood tests can show if your blood clots too easily and help your provider figure out why. These tests usually look for the following:
- Blood components. Several tests measure certain types of blood cells like platelets and chemical compounds, especially ones that affect clotting.
- Clot-formation markers. These are chemicals that typically only show up in your blood if you have a clot at the time. They can help healthcare providers confirm or rule out an active clot.
- Heart damage markers. An example of this is troponin, a protein in muscle cells. Your heart muscle cells contain a very specific type of troponin that doesn’t occur elsewhere in your body. Damage to your heart cells, such as from a heart attack, causes troponin to leak into your blood. Troponin tests can help confirm or rule out heart attacks, which often happen due to thrombosis. A blood clot in your lungs can also result in an elevated troponin due to increased strain on the heart because it pumps blood through the lungs.
Management and Treatment
How is thrombosis treated?
Thrombosis treatments include medications, minimally invasive procedures and surgeries. Your provider will tailor treatment to your needs.
Possible treatments include:
- Blood-thinners. These medications keep your blood from clotting too easily. They can’t get rid of an existing clot, but they can prevent it from growing. There are two classes of blood-thinners: antiplatelet drugs and anticoagulants.
- Thrombolytic therapy. Thrombolytic therapy uses medications to dissolve blood clots. Such “clot-busting drugs” are especially helpful for clots in critical areas. They serve as emergency treatment for heart attacks, strokes, and other thrombosis complications.
- Thrombectomy. One of the most direct ways to remove a clot is for a surgeon to access it and remove it. That’s what happens with thrombectomy. Surgeons use open or minimally invasive techniques.
You may also need additional treatments for complications of thrombosis. Your provider can explain what you might need and why it’s necessary.
How soon after treatment will I feel better?
Most people who receive treatment feel better as they’re treated, especially as blood returns to previously blocked areas. That can happen in minutes or hours, depending on the location and size of the clot and the specific treatments.
In cases where you had severe effects from a clot, like a heart attack or stroke, it may be a few days before you start feeling better. That’s especially true if you need surgery or more intensive procedures and care.
Your healthcare provider is the person who best understands your case. They can tell you more about what to expect in your specific circumstances.
Prevention
How can I prevent thrombosis?
When you know you’re at risk for clots, prevention is much easier. The best way to know about your risk is to get an annual physical (wellness visit or checkup). Your provider can detect many conditions that raise your risk for thrombosis long before clots form and offer guidance on prevention.
Your provider may recommend:
- Blood pressure medications. Over time, high blood pressure puts too much stress on the inside of your blood vessels. This kind of wear and tear can make it easier for blood clots to form and grow on your vessel walls. Blood pressure medications prevent clots by not giving them new places to form.
- Blood-thinning medications. These medications prevent your blood from clotting too easily. Providers use various types to both prevent and treat thrombosis.
- Cholesterol-lowering medications. Your cholesterol levels influence the buildup of plaque in your arteries, and plaque raises your risk for thrombosis. Lowering your cholesterol limits that buildup.
- Managing your weight with diet and exercise. Try to eat a heart-healthy diet (like the Mediterranean Diet). Plus, get enough exercise (150 minutes of moderate-intensity activity per week). Doing so can help you keep a weight that’s healthy for you.
- Moving around more. Sitting for long periods raises your risk for thrombosis. If your job keeps you sitting or standing for long periods, take short breaks. Even standing up and stretching for a couple of minutes can help. If you’re unable to stand up or move about due to health conditions or other circumstances, ask your provider for alternative ways to keep your blood moving with activity.
- Quitting tobacco use. Smoking and other forms of tobacco use (like vaping and smokeless tobacco) greatly increase your risk for thrombosis. Ask your provider for resources to help you quit. And if you don’t currently use tobacco, don’t start.
Outlook / Prognosis
What can I expect if I have this condition?
Early diagnosis and treatment can restore your blood flow and lower your chance of complications. If a complication (like a heart attack or stroke) leads to your diagnosis, your provider will treat that condition and do whatever possible to restore function to affected organs and tissues.
How long does thrombosis last?
It depends on the underlying cause, the treatments and how quickly you seek medical attention. Thrombosis can be short-lived with prompt treatment. However, the conditions that cause it may be chronic or lifelong. For example, blood clotting disorders that you’re born with may put you at risk for thrombosis throughout life. Your provider can help you manage underlying conditions to lower your risk.
What is the outlook for people with thrombosis?
Your outlook or prognosis depends on many factors, including:
- How quickly you seek care.
- Where the clot forms.
- Whether the clot stays in one place or travels in your bloodstream.
- Whether complications occur.
A clot that stays in place is a problem, but it’s usually less dangerous than a clot traveling in your bloodstream. The outlook for thrombosis can worsen when a free-floating clot ends up in a critical organ like your heart, brain or lungs.
Your provider can tell you more about your prognosis based on your individual situation.
Living With
How do I take care of myself?
If you’ve had thrombosis in the past or are at risk, it’s crucial to:
- Take your medications exactly as your provider tells you to. The risk of complications increases sharply if you suddenly stop taking medications that prevent thrombosis, especially blood-thinners. It’s also dangerous to take more than the recommended amount (such as double-dosing after forgetting to take a dose).
- See your provider regularly. Your provider will tell you how often you should come in for appointments. Go to all of your appointments so your provider can keep an eye on your condition.
- Make lifestyle changes. Ask your provider which changes are most important for you, and ask for resources to support you along the way.
- Connect with others. Talking with others who are in your shoes can help manage any worries or anxieties you might feel. Your provider can help you find communities where you can connect in-person or online.
When should I go to the ER?
Call 911 or your local emergency number if you have symptoms of thrombosis. Don’t delay. Thrombosis can very easily become a dangerous, life-threatening condition. The more minutes that pass, the greater the risk of complications.
A note from Cleveland Clinic
Thrombosis is a condition that can quickly become a life-threatening emergency. The most important thing you can do is try to prevent thrombosis. While you can’t always prevent it, knowing the symptoms can help you recognize when to seek immediate medical care.
If you’ve had thrombosis in the past, you may worry about what the future will bring. Share your questions and concerns with your provider. They’re your best source of information about what you can expect in your specific situation.