Book Appoinment
Testicular Cancer
Testicular cancer is the most common cancer affecting people assigned male at birth aged 15 to 35. The most common sign to look out for is a painless lump in your testicle. Testicular cancer that’s diagnosed and treated early has an excellent cure rate.
Overview
What is testicular cancer?
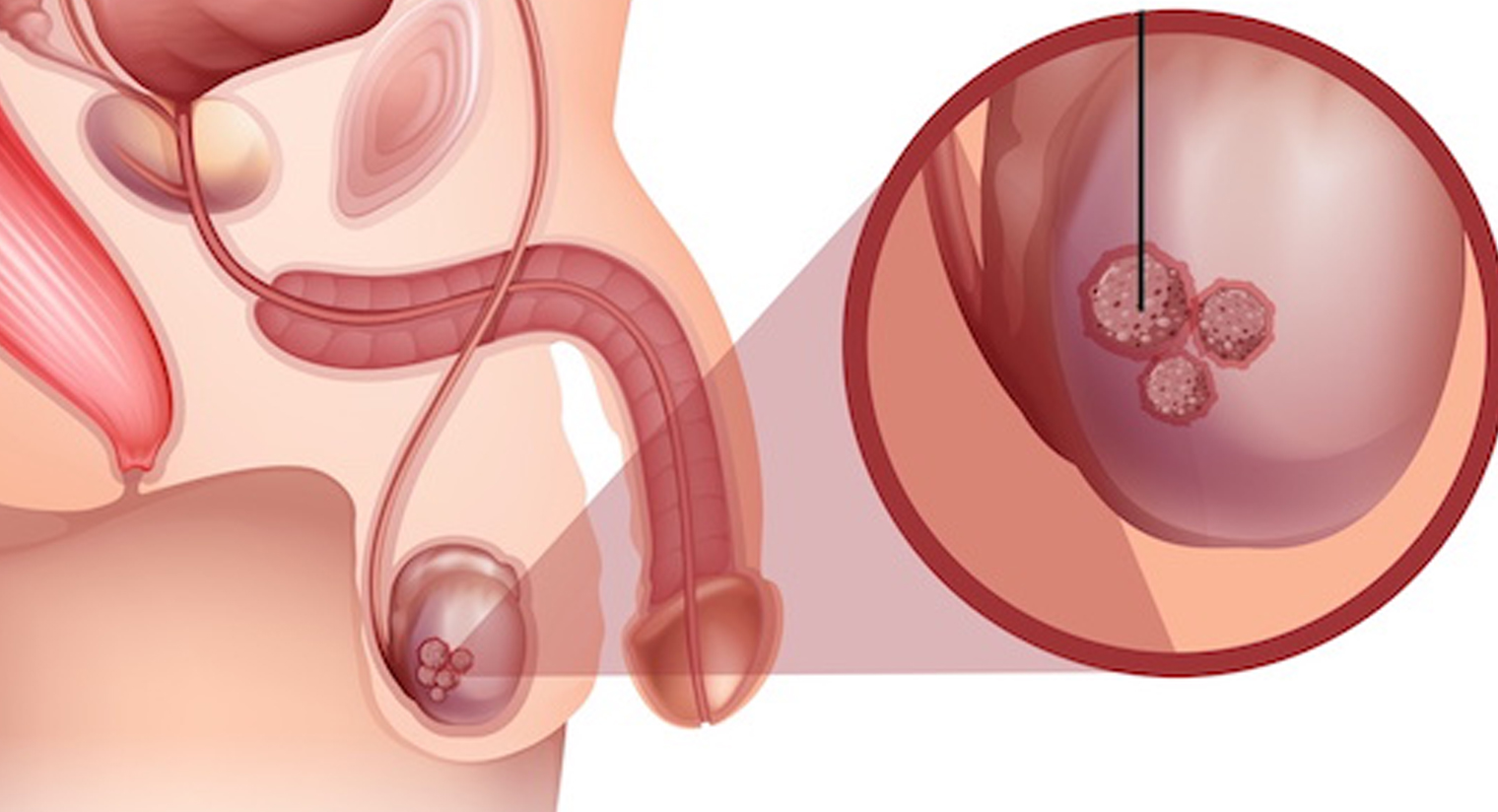
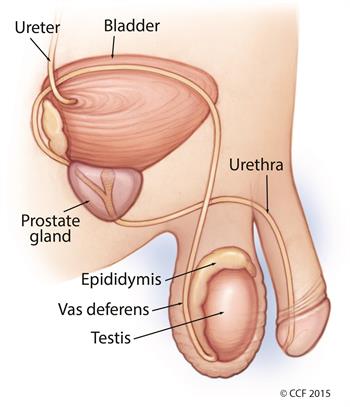
Testicular cancer forms when malignant (cancer) cells develop in the tissues of one or (less commonly) both testicles. Your testicles are two walnut-shaped sex glands that produce sperm and the hormone testosterone. They sit inside a sac of skin that lies below your penis called the scrotum.
Like any cancer, testicle cancer is a serious condition. Fortunately, testicular cancer is highly treatable and curable.
What are the types of testicular cancer?
About 90% of all testicular cancer arises from germ cells in your testicles that clump together to form a mass or tumor. Germ cells eventually develop into sperm. Two types of testicular cancer arise from germ cells.
- Semenoma: Slow-growing cancer that primarily affects people in their 40s or 50s.
- Non-seminoma: Cancer that grows more rapidly than seminomas. It mainly affects people in their late teens, 20s, and early 30s. There are four types of non-seminoma tumors. Each is named after the type of germ cell that makes up the tumor. Non-seminoma tumors include embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, and teratoma.
Some testicular cancer tumors consist of both seminoma and non-seminoma cells.
How common is testicular cancer?
Testicular cancer is rare, affecting only about 1 in 250 people with testicles in their lifetimes. Still, it’s the most common cancer among people assigned male at birth aged 15 to 35.
Symptoms and Causes
What are the signs and symptoms of testicular cancer?
The most common sign of testicular cancer is a painless lump in your testicle. Other symptoms include:
- Swelling or sudden fluid build-up in your scrotum.
- A lump or swelling in either testicle.
- A feeling of heaviness in your scrotum.
- Dull ache in your groin or lower abdomen.
- Pain or discomfort in your scrotum or a testicle.
- A shrinking testicle (testicular atrophy).
These symptoms can occur with other conditions, too, so don’t panic if you notice them. Still, schedule a visit with your provider to be sure. Delays in diagnosis allow cancer cells time to spread, making the disease harder to treat.
What causes testicular cancer?
Testicular cancer develops when cells multiply faster than usual, eventually forming a lump or tumor. Researchers aren’t sure what causes cells to behave this way. They do know that the cells that become testicular cancer are usually germ cells.
What are the risk factors for developing testicular cancer?
Several factors may increase your testicular cancer risk. Risk factors don’t cause testicular cancer, but they may increase its likelihood of developing.
Risk factors for testicular cancer include:
- Age: Testicular cancer most commonly affects people between ages 15 and 35.
- Undescended testicles: Testicles form in the abdomen of a fetus during pregnancy and usually drop into the scrotum before birth. Testicles that don’t drop are called undescended testicles and may require surgery. Being born with this condition may increase your testicular cancer risk even if you have surgery.
- Race and ethnicity: Testicular cancer is more common among non-Hispanic whites in the United States and Europe.
- Personal or family history: You may be more likely to develop testicular cancer if a biological parent or sibling had it. Certain inherited genetic conditions, like Klinefelter Syndrome, may also increase your risk. Having testicular cancer in one testicle increases your likelihood of developing a second cancer in the other testicle.
- Infertility: Some of the same factors that cause infertility may also be related to the development of testicular cancer. More research is needed to understand the connection.
Diagnosis and Tests
How is testicular cancer diagnosed?
Your provider may diagnose testicular cancer after investigating a lump or other change in your testicle you found during a self-exam. Sometimes testicular cancer gets diagnosed during a routine physical exam.
Common procedures and tests to help diagnose testicular cancer include:
- A physical exam and history: Your provider will ask about your symptoms and examine you closely to check for signs of testicular cancer. They may feel your testicles for lumps and inspect your lymph nodes for signs of cancer spread.
- Ultrasound: If your provider notices an abnormality during the exam, they’ll likely order an ultrasound. An ultrasound is a painless medical procedure that uses high-energy sound waves to create pictures of tissue inside your body.
- Inguinal orchiectomy and biopsy: If the ultrasound shows evidence of cancer, your provider will remove the affected testicle through an incision (cut) in your groin. A specialist will examine tissue from your testicle using a microscope to check for cancer cells.
Other tests may include:
- A serum tumor marker test: This procedure examines a blood sample to measure the amounts of certain substances linked to specific types of cancers. These substances are called tumor markers. The tumor markers that are often elevated in testicular cancer are alpha-fetoprotein (AFP), human chorionic gonadotropin (HCG or beta-HCG), and lactate dehydrogenase (LDH). Different types of tumors elevate different markers. For example, seminomas sometimes raise HCG but not AFP. Non-seminomas may raise AFP but not HCG. Elevated LDH levels may indicate cancer spread.
- CT scans, X-rays, and MRIs: A CT scan (or CAT scan) uses X-rays to form pictures of the inside of your body. Your provider may perform a CT scan of your abdomen and pelvis to see if your cancer’s spread to your abdominal organs. They may order a CT scan or standard X-ray to see if cancer’s spread to your lungs. If your provider suspects cancer has spread to your central nervous system (brain and spinal cord), you may get an MRI. An MRI uses magnets and radio waves to form pictures of the inside of your body.
What are the stages of testicular cancer?
Diagnosis also involves cancer staging. Staging provides important information that will guide treatment decisions, such as tumor size and whether the cancer’s spread.
- Stage 0: Abnormal cells have developed but are still inside the testicles where sperm cells start to develop. Stage 0 is also called germ cell neoplasia in situ (GCNIS).
- Stage I: Cancer is confined to the testicle, which may include nearby blood or lymph vessels. Tumor markers may or may not be elevated.
- Stage II: Cancer has spread to the lymph nodes in the back of your abdomen (also called the retroperitoneum) but not anywhere else. If you have cancer in your lymph nodes along with moderately or highly elevated tumor markers, then you’re in stage III rather than stage II.
- Stage III: Cancer has spread to lymph nodes beyond your abdomen or to an organ.
Management and Treatment
What are the treatments for testicular cancer?
Treatment depends on several factors, including your health, treatment preferences, cancer stage, and tumor type. Seminomas tend to grow more slowly and respond better to radiation therapy than non-seminomas. Both kinds of testicular cancer tumors respond well to chemotherapy treatments.
If testicular cancer involves both seminoma and non-seminoma tumors, your provider will treat it as a non-seminoma.
Surgery
Surgery to remove the cancerous testicle is the most common treatment for testicular cancer, regardless of cancer stage or tumor type. In some cases, your provider may also remove your lymph nodes.
- Radical inguinal orchiectomy: Your provider may perform orchiectomy (removing the testicle) to treat both seminoma and non-seminoma testicular cancers. During the procedure, your provider will make an incision into your groin to remove the testicle with the tumor. They’ll also close off blood vessels and lymphatic tissue to prevent the spread of cancer from the tumor site to the rest of your body.
- Retroperitoneal lymph node dissection (RPLND): Your provider may perform retroperitoneal lymph node dissection depending on your cancer’s stage and the tumor type. RPLND is more common with non-seminoma testicular cancers. During the procedure, your provider makes an incision into your abdomen and removes the lymph nodes behind your abdominal organs. RPLND may be used to treat cancer and may also be used for cancer staging.
Your provider may also perform surgery to remove tumors that have spread to your lungs or liver.
Radiation therapy
Radiation therapy uses high-dose X-rays to kill cancer cells. Radiation might be used after surgery to prevent the tumor from returning. Usually, radiation is limited to the treatment of seminomas.
Chemotherapy
Chemotherapy uses drugs such as cisplatin, bleomycin, and etoposide to kill cancer cells. Chemotherapy has improved the survival rate for people with both seminomas and non-seminomas. Depending on your cancer, you may receive chemotherapy instead of surgery. It may be used before an RPLND procedure or after a radical inguinal orchiectomy. Chemotherapy may also be used to treat cancer that’s returned (recurred) following remission.
Prevention
How can I prevent testicular cancer?
Testicular cancer isn’t preventable, but you can perform testicular self-exams (TSE) to identify changes in your testicles that you should bring to your provider’s attention. Your provider should know about lumps, nodules, hardness or a testicle that’s become bigger or smaller.
Many providers recommend performing a testicular self-exam monthly.
How do I perform a testicular self-exam to protect myself from testicular cancer?
You can complete a TSE in as little as two minutes. Many providers recommend performing a testicular self-exam monthly.
To do a self-exam, follow these steps.



- Do the exam after a warm shower or bath. The warmth relaxes the skin of your scrotum, making it easier to feel anything unusual.
- Use both hands to examine each testicle. Place your index and middle fingers underneath the testicle with your thumbs on top. Roll each testicle between your thumbs and fingers.
- Familiarize yourself with what’s normal. As you feel each testicle, you might notice a cord-like structure on top and in the back. This structure is called the epididymis. It stores and transports sperm. Don’t confuse it with a lump. It’s also normal for testicles to be slightly different sizes. Although the left and right testicles are often different sizes, each testicle should remain generally the same size.
- Feel for any lumps. Lumps can be pea-size or larger and are often painless. If you notice a lump, contact your healthcare provider.
If you notice a change in the size of your testicles or feel a lump, contact your healthcare provider.
You should also get a physical exam yearly.
Outlook / Prognosis
What is the prognosis (chance of recovery) for people with testicular cancer?
The prognosis for testicular cancer is excellent. This form of cancer is treated successfully in more than 95% of cases. Even people with unfavorable risk factors have, on average, a 50% chance of being cured.
Can testicular cancer be cured?
Testicular cancer is curable. While a cancer diagnosis is always serious, the good news about testicular cancer is that it is treated successfully in 95% of cases. If treated early, the cure rate rises to 98%.
Is testicular cancer fatal?
Testicular cancer can be fatal, but this is rare. Still, early detection makes a big difference in your prognosis. The earlier you see your provider and receive a diagnosis, the greater your chances of being cancer-free.
Living With
How do I take care of myself?
Many people wonder how having a testicle removed will impact their sex drive and fertility. One testicle is usually all you need to make enough testosterone to keep your hormone levels healthy and maintain your sex drive. You should still be able to get an erection and ejaculate.
In some instances, people with lymph nodes removed can get an erection but may have difficulty ejaculating.
Talk to your provider about any risks related to treatment. If you’re concerned about your fertility, sperm banking, or freezing your sperm for later, use may be an option.