Book Appoinment

Radiation Therapy
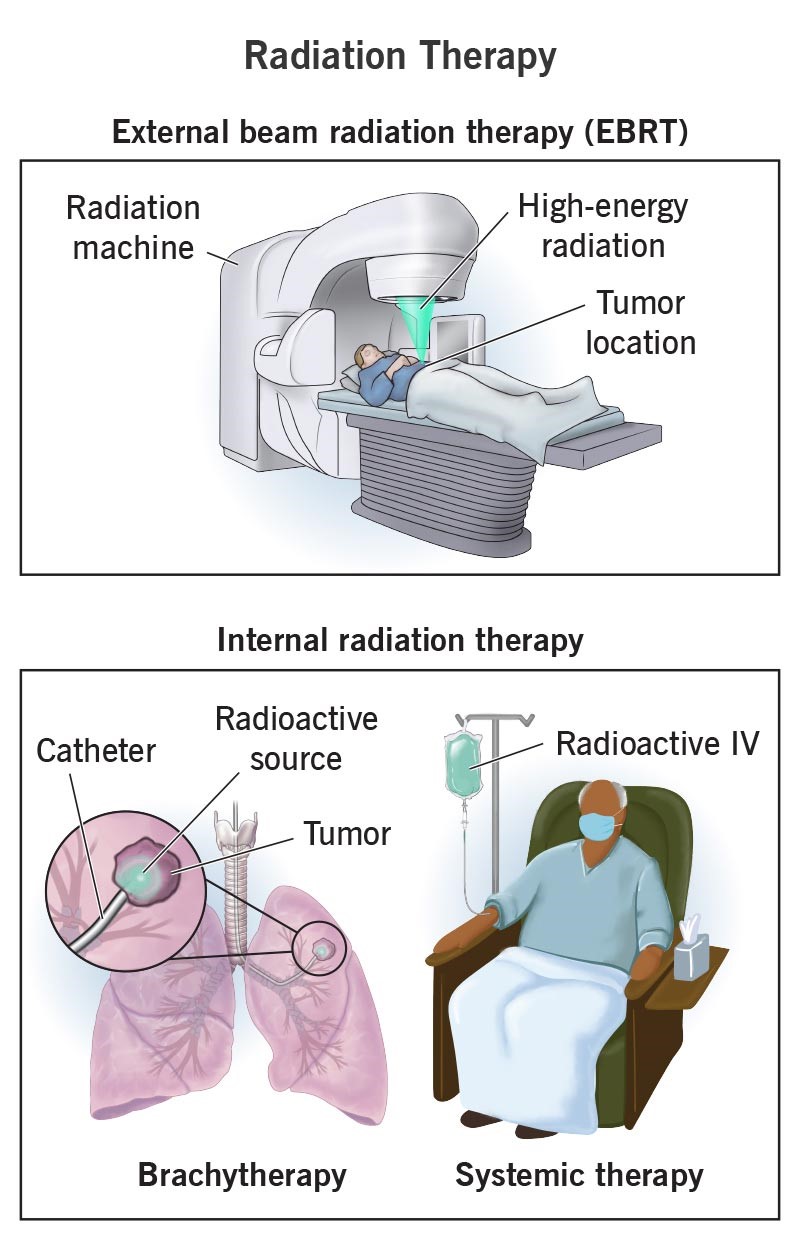
Radiation therapy, along with chemotherapy and surgery, is one of the most powerful tools we use to treat cancer. Radiation therapy includes the most common type, external beam radiation therapy (EBRT), and internal radiation therapy. Your radiation oncologist can recommend radiotherapy tailored to your condition and the kind of cancer you have.
In addition to its primary role in treating cancer, radiation therapy may also be used to alleviate symptoms caused by tumors, such as pain or obstruction. The treatment is often administered in a series of sessions, allowing for precise control over the dosage and targeting of the cancerous area.
What is radiation therapy (radiotherapy)?
Radiation therapy, also known as radiotherapy, is a widely used and effective cancer treatment that employs high-energy radiation, often in the form of X-rays, to destroy cancer cells. By damaging the DNA within these cells, radiation therapy prevents them from growing and dividing, ultimately leading to their death. This treatment can be used as a standalone approach, particularly for localized cancers, or it may be combined with other treatments such as surgery, chemotherapy, or immunotherapy to enhance overall effectiveness. Depending on the type and stage of cancer, radiation therapy can be used before surgery to shrink tumors, after surgery to eliminate any remaining cancer cells, or in conjunction with chemotherapy to improve treatment outcomes.
Radiation oncologists are specialists in administering radiation therapy. Your radiation oncologist will assess whether radiation therapy is suitable for you and, if so, will identify the most effective type for your specific cancer. They also create a customized treatment plan, carefully calculating the radiation dosage needed to destroy cancer cells while minimizing damage to surrounding healthy tissues.
Radiation therapy is a crucial cancer treatment that uses high-energy radiation to target and destroy cancer cells. This therapy works by damaging the DNA within cancer cells, preventing them from growing and multiplying. Radiation therapy can be used alone or in combination with other treatments, such as surgery and chemotherapy, to increase its effectiveness. Depending on the cancer type, stage, and location, radiation therapy may be administered externally, where a machine directs radiation beams at the tumor, or internally, where radioactive materials are placed inside or near the tumor. The treatment is carefully planned to maximize its impact on cancer cells while minimizing harm to surrounding healthy tissues, offering a highly targeted approach to cancer care.
Additionally, advancements in radiation technology have made the treatment more precise, reducing side effects and improving overall patient comfort.
What are the types of radiation therapy?
There are two main types of radiation therapy: external beam radiation therapy (EBRT) and internal radiation therapy. Both types work by destroying a cancer cell’s DNA. Without DNA instructions telling them to grow and multiply, cancer cells die and tumors shrink.
Internal radiation therapy
Internal radiation therapy places radiation inside of your body, close to cancer cells. It treats smaller tumors in your head, neck, breast, cervix, uterus or prostate.
You can receive internal radiation through a solid source or in liquid form:
- Brachytherapy implants a solid radioactive source, or “seed,” inside or beside a tumor. The source releases radiation to a small area to kill cancer cells. Some implants release low doses for longer periods (weeks). Others may release high doses for shorter periods (minutes). Some implants used in brachytherapy are temporary. Others stay in your body forever. Eventually, they stop releasing radiation.
- Systemic therapysends liquid radioactive material through your blood to find and destroy cancer cells. Some forms are swallowed. For others, you’ll receive an injection through a vein (IV). Treatments include radionuclide therapy (radioimmunotherapy). With radioimmunotherapy, a radioactive protein recognizes specific cancer cells, attaches to them and then releases radiation to kill them
Why is radiation therapy used?
Radiation therapy kills cancer cells, shrinks tumors and relieves cancer symptoms. It may be your only treatment, or it may be used to:
- Shrink tumors before other cancer treatments, like surgery (neo-adjuvant therapy)
- Destroy any remaining cancer cells after surgery (adjuvant therapy).
- Kill cancer cells that return after previous treatment.
Procedure Details
What happens before radiation therapy?
For internal radiation therapy, you may need a physical exam and imaging. Your radiation oncologist will explain how you can prepare for the day of the procedure based on how you’ll receive the radiation.
External beam radiation therapy (EBRT) involves a planning appointment called a simulation. Simulation is the treatment planning step that customizes your treatment.
Simulation involves:
- Getting in position. You’re positioned on a table exactly as you will be during treatment sessions. Your radiation therapy team may use a mold or mask to hold your body in place. They’ll ensure your alignment is correct. You may get temporary or permanent markings (tiny dots) that show which body parts should receive the radiation.
- Getting scans. You’ll receive a CT scan or an MRI that shows the tumor’s location. This information will help your care team customize X-rays that target a tumor while sparing healthy tissue.
Simulation allows your radiation oncologist to determine your radiation dosage and how you’ll receive it.
What happens during radiation therapy?
Internal radiation therapy usually happens in a special outpatient treatment room or in a hospital. Your radiation oncologist may insert the radiation implant using a small flexible tube called a catheter. For this treatment, you’ll receive anesthesia so you don’t feel pain or discomfort during the procedure. With the systemic form of internal radiation therapy, you’ll receive radioactive fluid through an IV.
With EBRT, you lie on a table, positioned as during simulation. The radiation machine moves around you but never touches you. A healthcare provider called a radiation therapist operates the machine from a separate room. You can speak to each other at any time using an intercom. The machine directs precise doses of radiation toward the tumor as it shifts positions. You won’t feel anything during treatment.
What happens after treatment?
With internal radiation therapy, you’ll typically go home after a short recovery the same day. Occasionally, you may need to stay in the hospital while your body sheds trace amounts of radiation. After systemic (IV) radiation therapy, you may secrete small amounts of radiation through body fluids, like sweat, pee and blood.
If you receive IV or permanent internal radiation therapy, there’s a small risk of exposing others to radiation. Follow your radiation therapy team’s guidance about how much contact you should have with others after radiotherapy.
You should be able to go about your regular daily activities before and after EBRT. There’s no risk of exposing others to radiation.
Risks / Benefits
What are radiation therapy side effects?
Most people receive radiation therapy spread out over multiple treatment sessions so they don’t receive the full dose all at once. The treatment schedule gives your healthy tissue time to recover between sessions. The healing time reduces side effects.
Still, you may experience unpleasant side effects that your radiation oncologist will help manage. Usually, these side effects only affect the part of your body receiving radiation directly.
Side effects may include:
- Fatigue.
- Nausea.
- Vomiting.
- Diarrhea.
- Headaches.
- Skin irritation.
- Dry, itchy scalp.
- Hair loss.
- Mouth sores.
- Pain when you swallow.
- Reduced appetite.
- A burning feeling in your throat or chest.
- Pain or a burning sensation when you pee.
- The need to pee frequently (often in small amounts).
- Abdominal bloating or cramps.
- Sense of urgency to have a bowel movement.
Ask your radiation oncologist what side effects to expect, given the kind of radiation therapy recommended for the kind of cancer you have.
What are the advantages of radiation therapy?
Radiation therapy is a reliable and effective cancer treatment that’s been around for over a century. Depending on the type of cancer you have, radiation therapy can destroy cancer cells and help other treatments work better. It’s also an important part of palliative care. It can ease cancer symptoms so that you live a fuller, more enjoyable life.
What are the risks or complications of this treatment?
Although radiation therapy effectively treats many types of cancer, it may also increase your likelihood of developing a different cancer in the future. For many people, the benefits of radiation therapy are worth the risk.
Weigh the benefits of treatment against potential risks with your radiation oncologist.
Recovery and Outlook
When can I get back to my normal routine?
Some people receiving radiation continue their routine with no problems. Others feel so sick that they need to take time out to rest. Many people don’t experience side effects until several weeks into treatment when more cells die.
Discuss best and worst-case scenarios with your radiation care provider as you plan your schedule around treatment.
When To Call the Doctor
When should I see my radiation care provider?
Your radiation care provider should know about any side effects you’re experiencing, especially those that interfere with your quality of life. Depending on your treatment response, your provider may need to adjust your dosage, change your treatment schedule or try a different type of treatment.